Improve your health
Improve your health
Improve your health
18. Januar 2026
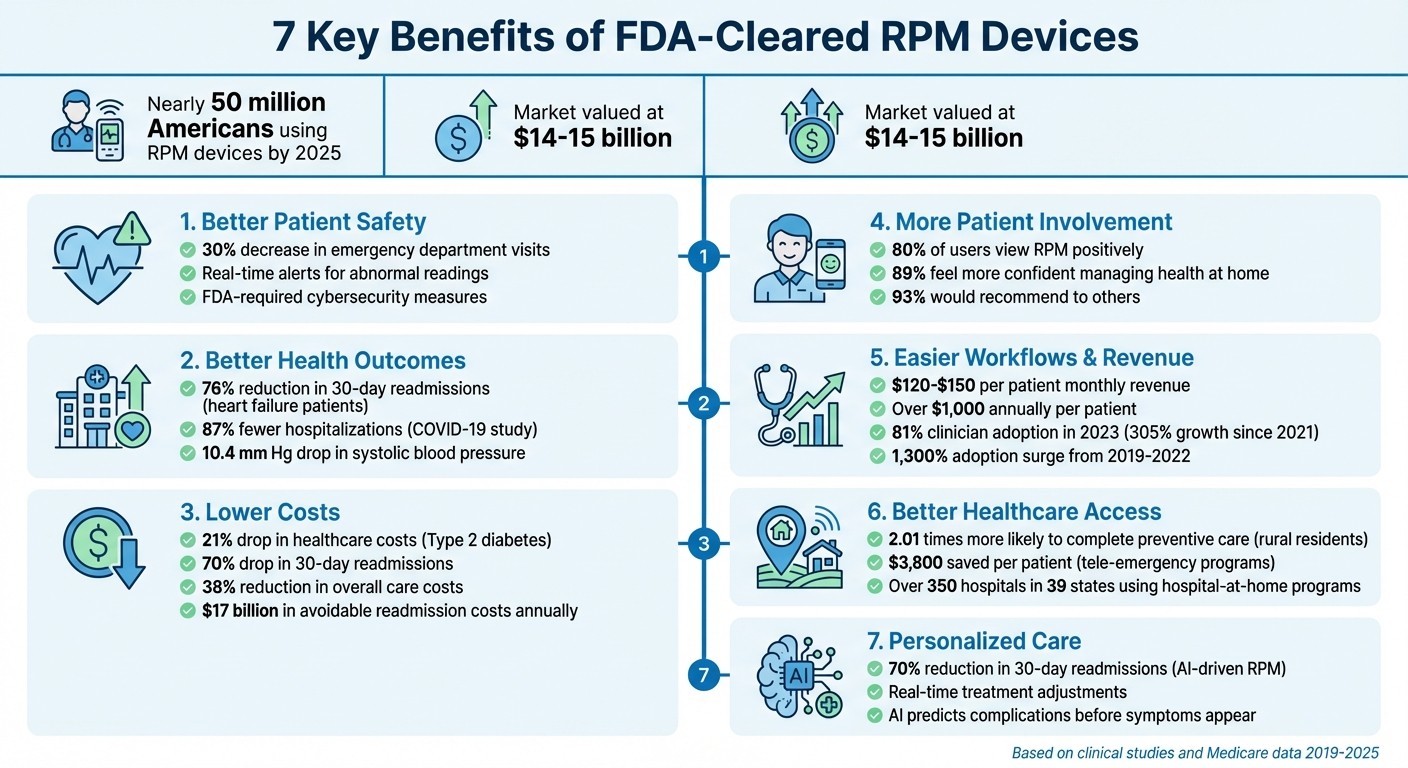
Key Benefits of FDA-Cleared RPM Devices


Remote Patient Monitoring (RPM) devices approved by the FDA are transforming healthcare by offering reliable, medical-grade tools to track vital signs like blood pressure, glucose levels, and oxygen saturation. These devices provide accurate data, enable early intervention, and reduce hospital visits - all while supporting patient care from home. Here's what you need to know:
Continuous Monitoring: Tracks vital signs in real time, helping detect issues early and improving patient safety.
Improved Health Outcomes: Reduces hospital readmissions and enhances chronic disease management.
Cost Savings: Cuts healthcare expenses by reducing emergency visits and hospital stays.
Patient Engagement: Empowers individuals to manage their health with real-time data and actionable insights.
Provider Efficiency: Simplifies workflows and creates new revenue opportunities through Medicare reimbursement.
Expanded Access: Brings healthcare to rural and underserved areas, eliminating barriers like travel.
Personalized Care: Uses real-time data for tailored treatment decisions, supported by AI-driven insights.
By 2025, nearly 50 million Americans were using RPM devices, with the market valued at $14–15 billion. These tools are reshaping healthcare by making it more accessible, efficient, and data-driven.
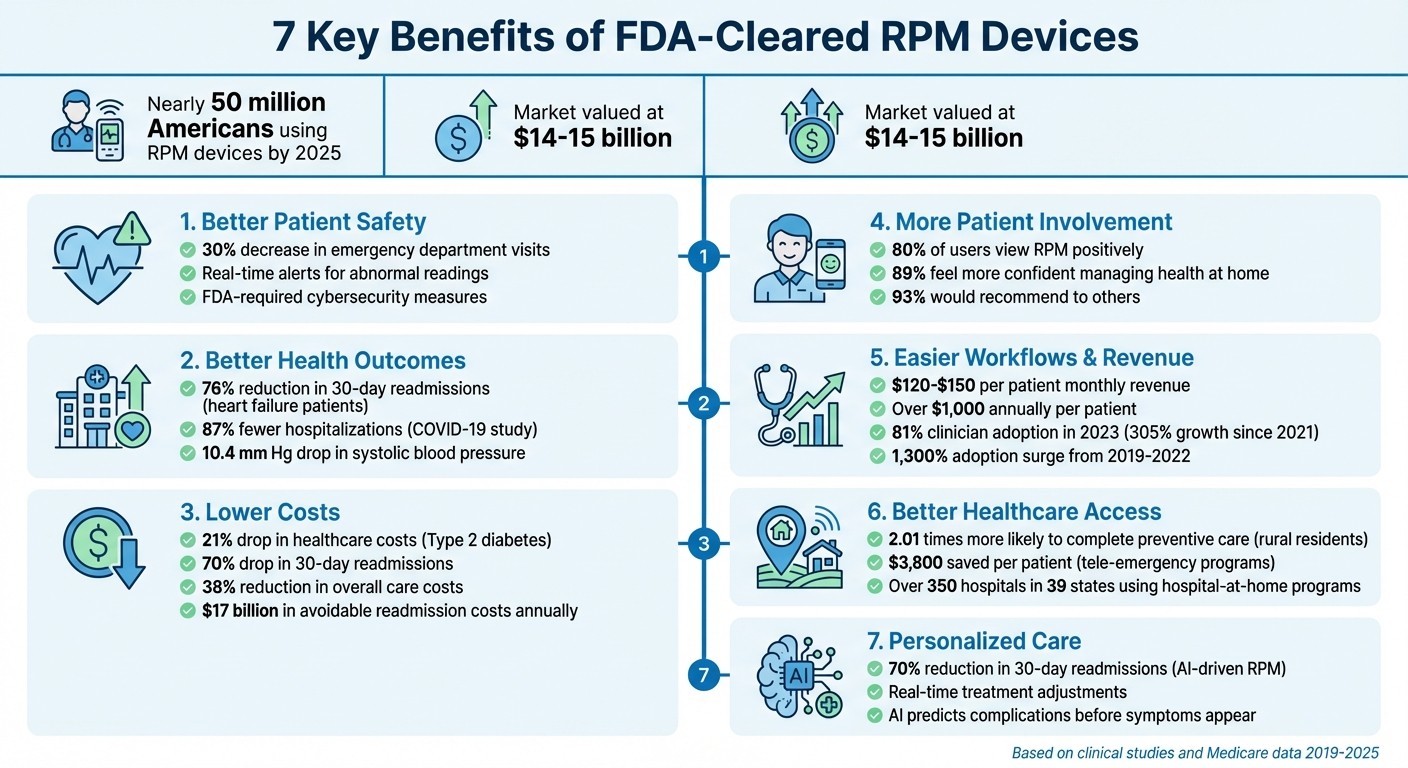
7 Key Benefits of FDA-Cleared Remote Patient Monitoring Devices
Biobeat - First and Only Company with FDA-Cleared Cuffless RPM to Screen Up to 13 Health Metrics
1. Better Patient Safety with Continuous Monitoring
FDA-cleared remote patient monitoring (RPM) devices are designed to keep patients safer by continuously tracking vital signs and catching potential issues early. Unlike consumer-grade fitness trackers, these medical-grade devices go through extensive testing to ensure they provide accurate clinical measurements. They monitor key metrics like heart rate, blood pressure, and oxygen levels, meeting strict FDA requirements. For example, manufacturers must validate their devices for specific groups, such as testing a step-counting algorithm tailored for Parkinson’s patients [7].
One of the standout features of RPM devices is their ability to send automated alerts when abnormal readings occur - like a sudden drop in oxygen levels or an irregular heartbeat. These alerts enable healthcare providers to respond quickly and prevent complications. A study by the Mayo Clinic on high-risk COVID-19 patients demonstrated the impact of RPM: patients using these devices had fewer emergency room visits, lower ICU admissions, and reduced mortality rates [4]. Another example shows organizations using RPM systems with real-time trending data saw a 30% decrease in emergency department visits among monitored patients [6]. However, the effectiveness of these alerts depends heavily on the reliability and integrity of the devices themselves.
To ensure accuracy and protect patient data, the FDA enforces strict cybersecurity measures and requires devices to pass wireless coexistence testing. Standards like ANSI C63.27 help prevent data loss or interference from nearby wireless equipment [1]. This is crucial because any unauthorized access or disruption could compromise patient safety [9].
"The most important part of RPM is providing good education to the patients about the devices, and what they should do when they get particularly concerning readings." - Dr. Colton Hood, Assistant Professor of Emergency Medicine, George Washington University [5]
For RPM to be effective, providers need to set personalized alert thresholds and establish clear response protocols. Proper patient education is equally important - simple steps like warming fingers before using a pulse oximeter can help reduce false readings [5].
2. Better Health Outcomes and Fewer Hospital Stays
FDA-cleared remote patient monitoring (RPM) devices are transforming healthcare by enabling early detection and timely intervention. By continuously tracking vital signs - like rising blood pressure or dropping oxygen levels - these devices help healthcare teams catch potential issues before they escalate into emergencies. This proactive approach not only reduces hospital readmissions but also improves the management of chronic conditions such as heart failure, COPD, and hypertension.
The numbers speak for themselves. Clinical studies show that RPM can dramatically cut readmissions. For instance, heart failure patients have seen reductions in 30-day readmissions by as much as 76%. One standout example is a UMass Memorial Health program, which achieved a 50% drop in readmissions by using an IoT network that linked blood pressure monitors and heart rate sensors to real-time clinical dashboards [10][11]. Meanwhile, a COVID-19 study in Cleveland, Ohio, revealed that patients monitored remotely after hospital discharge had 87% fewer hospitalizations and 77% fewer deaths compared to those not using RPM technology [12].
RPM devices also deliver measurable results in managing chronic diseases. A 12-month study found that patients using RPM saw a 10.4 mm Hg drop in systolic blood pressure, compared to just a 4.7 mm Hg decrease in the control group [14]. Practices with high RPM usage reported 9.3% fewer acute care visits related to hypertension [15]. Beyond cardiovascular health, RPM alerts have been linked to a 9.6% average reduction in hospitalizations and a 3% decrease in all-cause mortality [8].
"The ability to capture patient-generated health data with digital health technologies in near real time increases the capacity for early detection of adverse health trends, early intervention, and rapid response." - Tufia C. Haddad, Department of Oncology, Mayo Clinic [13]
The financial impact is equally compelling. In the U.S., nearly 20% of Medicare beneficiaries are readmitted within 30 days of discharge, leading to about $17 billion in avoidable costs annually [10]. With the average hospital readmission costing $15,200 [10], RPM devices offer a practical way to improve outcomes while cutting expenses. They also shorten hospital stays by an average of one day [10], freeing up vital resources and allowing patients to recover more comfortably at home.
3. Lower Costs for Patients and Healthcare Systems
FDA-cleared remote patient monitoring (RPM) devices are helping to cut healthcare costs by moving care from pricey hospital settings into patients' homes. These devices can catch early warning signs, like sudden spikes in blood pressure, allowing for timely intervention before a situation escalates into an emergency. For patients with chronic conditions such as heart failure, diabetes, or hypertension, this proactive care approach not only improves outcomes but also significantly reduces the financial burden tied to emergency treatments.
The numbers speak for themselves. A study on Type 2 diabetes patients using RPM lifestyle education software found a 21% drop in healthcare costs within one to two years of follow-up [16]. For heart failure patients, telemonitoring over 24 months led to 44% lower odds of being readmitted within 30 days and 38% lower odds within 90 days, translating to an 11% cost reduction for payors [17]. Some healthcare organizations have even reported a 30% decrease in emergency room visits for patients using RPM systems [6].
Patients also benefit financially. With fewer trips to the doctor and reduced office-visit copays, RPM can lower out-of-pocket expenses [17][18]. Many private insurers and Medicare cover RPM services, often leaving patients with no out-of-pocket costs. When copays are required, they typically average around $25 per month [17][18].
Healthcare providers see financial advantages as well. Medicare reimbursement for RPM services ranges from $120 to $150 per patient each month, which can add up to over $1,000 annually per patient [6]. Between 2019 and 2021, Medicare payments for RPM surged from $5.5 million to more than $101 million - a 19-fold increase [12]. In 2023, a health system using FDA-cleared RPM solutions reported a 70% drop in 30-day readmissions and a 38% reduction in overall care costs [6]. These financial gains highlight the dual value of RPM: better patient care and smarter cost management.
The growing adoption of hospital-at-home models is another way RPM is driving savings. By late 2024, more than 350 hospitals across 39 states had implemented the "Acute Hospital Care at Home" program under a CMS waiver. A report to Congress showed that this RPM-enabled inpatient care at home resulted in lower mortality rates and reduced overall costs compared to traditional hospital stays [6]. With continuous monitoring, RPM helps cut down on costly readmissions, emergency visits, and extended hospitalizations [8].
4. More Patient Involvement in Their Own Care
FDA-cleared remote patient monitoring (RPM) devices are transforming healthcare by giving patients real-time access to their health data. This technology encourages active self-care, allowing individuals to see how daily habits - like eating or exercising - impact their health. Take, for instance, a continuous glucose monitor: it updates blood sugar levels every few minutes, enabling diabetics to see immediate results from their meals or workouts. This instant feedback empowers patients to make adjustments in real time, rather than waiting weeks for follow-up appointments.
Patients are embracing these tools with enthusiasm. A survey found that 80% of users view the integration of RPM into medical care positively [6]. In a study conducted by the Mayo Clinic, 89% of participants reported feeling more confident managing their health at home with RPM, and 93% said they would recommend it to others [12]. These devices do more than just gather data - they help patients understand their health metrics and take proactive steps to improve them. This shift naturally supports a more collaborative approach to care.
"Digital tools are giving providers a more holistic view of patient health through access to data and giving patients more control over their health." - FDA [19]
Real-time data sharing also enhances communication between patients and healthcare providers. Instead of relying on memory or sporadic self-reports during office visits, patients can analyze their data trends and come to appointments with specific questions. This collaborative approach has already shown success in conditions like hypertension and Type 2 diabetes, where real-time data allows for immediate medication adjustments without the need for clinic visits [6].
In addition to fostering collaboration, RPM devices bring convenience to the forefront. Nearly half of patients (43%) cite convenience as a major benefit [6]. Features like automated reminders improve medication adherence, while continuous monitoring promotes accountability without requiring frequent trips to the doctor. The impact is clear: RPM interventions have led to better adherence to both medication and lifestyle changes [8]. Digital platforms such as Healify take it a step further by using continuous data to offer personalized coaching and actionable recommendations, deepening patient engagement in their own care journey.
5. Easier Workflows and New Revenue for Providers
Beyond saving costs and improving patient outcomes, Remote Patient Monitoring (RPM) devices are transforming how healthcare providers manage their workflows while unlocking new revenue opportunities. These FDA-cleared devices simplify processes by automatically uploading vital data - like blood pressure, glucose levels, and oxygen saturation - directly to secure cloud platforms or Electronic Health Records (EHRs) such as Epic and Oracle Cerner. Advanced RPM systems use algorithms for exception-based monitoring, flagging only abnormal readings. This allows clinical staff to focus their attention where it’s needed most, making operations more efficient and productive.
"Clinicians... need automated tools that can 'learn' from repeated exposure to vast amounts of data and surface only what's truly valuable." - Margaret Lindquist, Content Strategist, Oracle Health [4]
RPM doesn’t just streamline workflows - it generates substantial revenue for providers. Medicare RPM services allow providers to earn around $120–$150 per patient each month, adding up to over $1,000 annually per patient [6]. This revenue is tied to specific CPT codes, including:
99453: Covers initial setup and patient education.
99454: Covers monthly device supply and data transmission (requires at least 16 days of data in a 30-day period).
99457: Covers the first 20 minutes of clinical staff time for monitoring and communication.
99458: Covers each additional 20 minutes of clinical staff time [6][21].
One key advantage of RPM is that it doesn’t require direct physician involvement for routine monitoring. Under Medicare guidelines, clinical staff - like nurses or medical assistants - can handle monitoring and patient communication under general supervision [21]. This frees up physicians to focus on more complex cases, enhancing overall efficiency. Adoption of RPM by clinicians reached 81% in 2023, marking a 305% growth since 2021 [6]. Furthermore, 77% of clinicians believe RPM-enabled care will surpass traditional inpatient care within the next five years [6].
"RPM adoption from 2019 to 2022 surged ~1,300% in the U.S., a reflection of how quickly virtual care has been embraced in both chronic and acute settings." - Adrien Laurent, Content Lead [6]
To maximize benefits, providers should partner with RPM vendors that integrate seamlessly with existing systems via FHIR standards. This ensures patient data automatically populates into charts, reducing manual work. Platforms that track the 16-day data transmission requirement also help providers maintain billing compliance effortlessly. Some providers even collaborate with full-service RPM vendors offering 24/7 monitoring centers staffed by licensed nurses. These teams handle initial data reviews and escalate critical issues to physicians only when necessary. By aligning with FDA-cleared standards, these integrated platforms not only improve workflow efficiency but also enhance the broader care ecosystem.
6. Better Healthcare Access for Rural and Underserved Areas
For people living in rural areas, accessing healthcare often means long drives to the nearest clinic or hospital, which can delay necessary care. FDA-cleared remote patient monitoring (RPM) devices are changing that by bringing care directly into patients' homes. This approach removes the need for extensive travel, making both primary and specialty care more accessible. It's a game-changer for overcoming the challenges of geographic isolation.
In 2020, rural residents who utilized telemedicine and RPM were 2.01 times more likely to complete preventive care visits or services in 2021 [23]. This is a big deal because rural populations have historically struggled to access preventive healthcare due to transportation and distance issues. Additionally, tele-emergency programs in rural hospitals have proven to be cost-effective, saving approximately $3,800 per patient by avoiding unnecessary transfers to urban facilities [22].
"Telemedicine fosters a collaboration that reduces the feelings of isolation that physicians may experience when they go to practice in a small town. With telemedicine, it's like having one foot in the city but being able to live and practice out in a rural area." - Dr. Wilbur Hitt, Healthcare Provider [22]
FDA-cleared RPM devices, such as blood pressure cuffs, glucometers, pulse oximeters, and ECG patches, are bridging gaps in healthcare access. These devices automatically send accurate, medical-grade data to healthcare providers. This allows doctors to adjust medications, conduct virtual follow-ups, and step in early if readings are outside safe ranges - all without the patient needing to leave home [3][4]. By catching potential issues early, this approach helps prevent complications that could otherwise lead to emergency room visits or hospital stays, offering a vital lifeline for rural communities.
7. Personalized Care Based on Patient Data
FDA-cleared remote patient monitoring (RPM) devices are transforming healthcare by continuously collecting vital signs such as blood pressure, glucose levels, heart rhythms, and oxygen saturation. This steady flow of information offers a real-world glimpse into a patient’s health, far beyond the limited snapshot provided during a clinical visit [7]. It’s like having a window into how patients are doing in their everyday lives, not just when they’re in the doctor’s office.
The data is transmitted in real time, allowing healthcare providers to make immediate, personalized treatment decisions [3][20]. For instance, if a patient’s blood pressure stays elevated for several days, their provider can adjust medications right away instead of waiting weeks for the next appointment. These persistent trends enable providers to respond more quickly and effectively [3]. On top of that, advanced analytics take this personalization to the next level by refining treatment strategies based on the patterns revealed.
Artificial intelligence (AI) and machine learning are leading the charge in enhancing this level of care. In 2023, Biofourmis used FDA-approved algorithms to predict heart failure exacerbations before patients even noticed symptoms [6]. One health system that adopted this AI-driven RPM approach saw remarkable results: a 70% reduction in 30-day hospital readmissions and a 38% decrease in the overall cost of care [6]. AI tools also analyze continuous data to pick up early warning signs - like small changes in heart rhythm or fluid retention - that might otherwise go unnoticed [6][8].
"Digital tools are giving providers a more holistic view of patient health through access to data and giving patients more control over their health." - FDA [19]
AI-powered platforms like Healify take this personalization even further. By analyzing data from wearables, biometrics, and lifestyle factors, these tools deliver real-time, tailored health recommendations. This helps both patients and providers zero in on what truly matters, turning raw data into actionable insights. The continuous data collection enabled by RPM ensures that care is real-world and tailored to each individual’s unique needs [3].
Conclusion
FDA-cleared remote patient monitoring (RPM) devices are transforming healthcare by providing continuous, real-time data. This allows for earlier detection of potential issues, quicker treatment adjustments, and fewer hospital readmissions[4][24]. For patients, RPM devices mean fewer trips to the clinic, better management of chronic conditions, and the peace of mind that comes with consistent monitoring[4][24].
The numbers speak for themselves. Recent data shows a 19-fold increase in RPM reimbursement, signaling rapid adoption by millions of patients and healthcare providers[4][6]. This growing use of RPM technology paves the way for AI-driven advancements that promise to refine care even further.
Artificial intelligence is already adding a powerful edge to RPM. AI-guided platforms have been shown to significantly cut hospital readmissions and reduce overall care costs[6]. For example, platforms like Healify use RPM data to deliver personalized, actionable health insights, moving closer to the goal of fully tailored care.
The FDA is also playing a pivotal role in supporting this progress. Its TEMPO pilot program, launched in January 2026, highlights a commitment to driving digital health innovations aimed at improving patient outcomes[2]. Margaret Lindquist of Oracle Health captured this sentiment well:
"The World Health Organization identifies remote patient monitoring as one of a handful of healthcare delivery models with the potential to vastly improve global health outcomes"[4].
These FDA-cleared devices are laying the foundation for a new era of personalized, AI-enhanced healthcare that has the potential to improve lives on a measurable scale.
FAQs
What makes FDA-cleared remote patient monitoring (RPM) devices accurate and safe for patients?
FDA-cleared remote patient monitoring (RPM) devices focus on delivering precise measurements while ensuring patient safety. These devices are subjected to thorough validation and calibration to guarantee their sensors consistently provide dependable data. On top of that, they include strong cybersecurity features, such as encrypted data transmission and secure software, to safeguard sensitive health information.
To promote safer use, FDA guidelines emphasize proper device setup and educating patients on how to use them effectively. This approach helps users operate the devices correctly, resulting in more reliable readings and improved health management.
What financial advantages do FDA-cleared RPM devices offer for patients and healthcare providers?
Remote patient monitoring (RPM) devices that are cleared by the FDA offer a practical way for patients to cut down on healthcare expenses. By helping avoid expensive hospital stays or emergency room visits, these devices can make a real difference in managing costs.
For healthcare providers, RPM devices open the door to Medicare reimbursement opportunities while also contributing to lower overall expenses within the healthcare system.
With their focus on proactive care and early intervention, RPM devices do more than just improve health outcomes - they also ease the financial strain on patients and the system as a whole.
How do remote patient monitoring devices improve healthcare access in rural and underserved areas?
Remote patient monitoring (RPM) devices empower patients to track vital health metrics - like blood pressure, glucose levels, weight, and oxygen saturation - right from the comfort of their homes. These devices securely transmit data to healthcare providers, cutting out the need for long, often inconvenient trips to clinics. This is especially crucial in rural or underserved areas where access to healthcare providers can be limited.
Since these devices are FDA-cleared, they’re trusted for their reliability and accuracy. Medicare also supports RPM services, covering costs when patients share at least 16 readings within a 30-day period. This makes RPM a practical and affordable way to improve healthcare access, manage chronic conditions, and keep patients actively involved in their health.
Healify takes RPM a step further by combining it with AI-powered health coaching. Its virtual coach is available 24/7, offering personalized advice and real-time support. For patients in remote areas, this means staying on top of their health and receiving guidance, even without frequent in-person visits to a doctor’s office.
Related Blog Posts
Remote Patient Monitoring (RPM) devices approved by the FDA are transforming healthcare by offering reliable, medical-grade tools to track vital signs like blood pressure, glucose levels, and oxygen saturation. These devices provide accurate data, enable early intervention, and reduce hospital visits - all while supporting patient care from home. Here's what you need to know:
Continuous Monitoring: Tracks vital signs in real time, helping detect issues early and improving patient safety.
Improved Health Outcomes: Reduces hospital readmissions and enhances chronic disease management.
Cost Savings: Cuts healthcare expenses by reducing emergency visits and hospital stays.
Patient Engagement: Empowers individuals to manage their health with real-time data and actionable insights.
Provider Efficiency: Simplifies workflows and creates new revenue opportunities through Medicare reimbursement.
Expanded Access: Brings healthcare to rural and underserved areas, eliminating barriers like travel.
Personalized Care: Uses real-time data for tailored treatment decisions, supported by AI-driven insights.
By 2025, nearly 50 million Americans were using RPM devices, with the market valued at $14–15 billion. These tools are reshaping healthcare by making it more accessible, efficient, and data-driven.
7 Key Benefits of FDA-Cleared Remote Patient Monitoring Devices
Biobeat - First and Only Company with FDA-Cleared Cuffless RPM to Screen Up to 13 Health Metrics
1. Better Patient Safety with Continuous Monitoring
FDA-cleared remote patient monitoring (RPM) devices are designed to keep patients safer by continuously tracking vital signs and catching potential issues early. Unlike consumer-grade fitness trackers, these medical-grade devices go through extensive testing to ensure they provide accurate clinical measurements. They monitor key metrics like heart rate, blood pressure, and oxygen levels, meeting strict FDA requirements. For example, manufacturers must validate their devices for specific groups, such as testing a step-counting algorithm tailored for Parkinson’s patients [7].
One of the standout features of RPM devices is their ability to send automated alerts when abnormal readings occur - like a sudden drop in oxygen levels or an irregular heartbeat. These alerts enable healthcare providers to respond quickly and prevent complications. A study by the Mayo Clinic on high-risk COVID-19 patients demonstrated the impact of RPM: patients using these devices had fewer emergency room visits, lower ICU admissions, and reduced mortality rates [4]. Another example shows organizations using RPM systems with real-time trending data saw a 30% decrease in emergency department visits among monitored patients [6]. However, the effectiveness of these alerts depends heavily on the reliability and integrity of the devices themselves.
To ensure accuracy and protect patient data, the FDA enforces strict cybersecurity measures and requires devices to pass wireless coexistence testing. Standards like ANSI C63.27 help prevent data loss or interference from nearby wireless equipment [1]. This is crucial because any unauthorized access or disruption could compromise patient safety [9].
"The most important part of RPM is providing good education to the patients about the devices, and what they should do when they get particularly concerning readings." - Dr. Colton Hood, Assistant Professor of Emergency Medicine, George Washington University [5]
For RPM to be effective, providers need to set personalized alert thresholds and establish clear response protocols. Proper patient education is equally important - simple steps like warming fingers before using a pulse oximeter can help reduce false readings [5].
2. Better Health Outcomes and Fewer Hospital Stays
FDA-cleared remote patient monitoring (RPM) devices are transforming healthcare by enabling early detection and timely intervention. By continuously tracking vital signs - like rising blood pressure or dropping oxygen levels - these devices help healthcare teams catch potential issues before they escalate into emergencies. This proactive approach not only reduces hospital readmissions but also improves the management of chronic conditions such as heart failure, COPD, and hypertension.
The numbers speak for themselves. Clinical studies show that RPM can dramatically cut readmissions. For instance, heart failure patients have seen reductions in 30-day readmissions by as much as 76%. One standout example is a UMass Memorial Health program, which achieved a 50% drop in readmissions by using an IoT network that linked blood pressure monitors and heart rate sensors to real-time clinical dashboards [10][11]. Meanwhile, a COVID-19 study in Cleveland, Ohio, revealed that patients monitored remotely after hospital discharge had 87% fewer hospitalizations and 77% fewer deaths compared to those not using RPM technology [12].
RPM devices also deliver measurable results in managing chronic diseases. A 12-month study found that patients using RPM saw a 10.4 mm Hg drop in systolic blood pressure, compared to just a 4.7 mm Hg decrease in the control group [14]. Practices with high RPM usage reported 9.3% fewer acute care visits related to hypertension [15]. Beyond cardiovascular health, RPM alerts have been linked to a 9.6% average reduction in hospitalizations and a 3% decrease in all-cause mortality [8].
"The ability to capture patient-generated health data with digital health technologies in near real time increases the capacity for early detection of adverse health trends, early intervention, and rapid response." - Tufia C. Haddad, Department of Oncology, Mayo Clinic [13]
The financial impact is equally compelling. In the U.S., nearly 20% of Medicare beneficiaries are readmitted within 30 days of discharge, leading to about $17 billion in avoidable costs annually [10]. With the average hospital readmission costing $15,200 [10], RPM devices offer a practical way to improve outcomes while cutting expenses. They also shorten hospital stays by an average of one day [10], freeing up vital resources and allowing patients to recover more comfortably at home.
3. Lower Costs for Patients and Healthcare Systems
FDA-cleared remote patient monitoring (RPM) devices are helping to cut healthcare costs by moving care from pricey hospital settings into patients' homes. These devices can catch early warning signs, like sudden spikes in blood pressure, allowing for timely intervention before a situation escalates into an emergency. For patients with chronic conditions such as heart failure, diabetes, or hypertension, this proactive care approach not only improves outcomes but also significantly reduces the financial burden tied to emergency treatments.
The numbers speak for themselves. A study on Type 2 diabetes patients using RPM lifestyle education software found a 21% drop in healthcare costs within one to two years of follow-up [16]. For heart failure patients, telemonitoring over 24 months led to 44% lower odds of being readmitted within 30 days and 38% lower odds within 90 days, translating to an 11% cost reduction for payors [17]. Some healthcare organizations have even reported a 30% decrease in emergency room visits for patients using RPM systems [6].
Patients also benefit financially. With fewer trips to the doctor and reduced office-visit copays, RPM can lower out-of-pocket expenses [17][18]. Many private insurers and Medicare cover RPM services, often leaving patients with no out-of-pocket costs. When copays are required, they typically average around $25 per month [17][18].
Healthcare providers see financial advantages as well. Medicare reimbursement for RPM services ranges from $120 to $150 per patient each month, which can add up to over $1,000 annually per patient [6]. Between 2019 and 2021, Medicare payments for RPM surged from $5.5 million to more than $101 million - a 19-fold increase [12]. In 2023, a health system using FDA-cleared RPM solutions reported a 70% drop in 30-day readmissions and a 38% reduction in overall care costs [6]. These financial gains highlight the dual value of RPM: better patient care and smarter cost management.
The growing adoption of hospital-at-home models is another way RPM is driving savings. By late 2024, more than 350 hospitals across 39 states had implemented the "Acute Hospital Care at Home" program under a CMS waiver. A report to Congress showed that this RPM-enabled inpatient care at home resulted in lower mortality rates and reduced overall costs compared to traditional hospital stays [6]. With continuous monitoring, RPM helps cut down on costly readmissions, emergency visits, and extended hospitalizations [8].
4. More Patient Involvement in Their Own Care
FDA-cleared remote patient monitoring (RPM) devices are transforming healthcare by giving patients real-time access to their health data. This technology encourages active self-care, allowing individuals to see how daily habits - like eating or exercising - impact their health. Take, for instance, a continuous glucose monitor: it updates blood sugar levels every few minutes, enabling diabetics to see immediate results from their meals or workouts. This instant feedback empowers patients to make adjustments in real time, rather than waiting weeks for follow-up appointments.
Patients are embracing these tools with enthusiasm. A survey found that 80% of users view the integration of RPM into medical care positively [6]. In a study conducted by the Mayo Clinic, 89% of participants reported feeling more confident managing their health at home with RPM, and 93% said they would recommend it to others [12]. These devices do more than just gather data - they help patients understand their health metrics and take proactive steps to improve them. This shift naturally supports a more collaborative approach to care.
"Digital tools are giving providers a more holistic view of patient health through access to data and giving patients more control over their health." - FDA [19]
Real-time data sharing also enhances communication between patients and healthcare providers. Instead of relying on memory or sporadic self-reports during office visits, patients can analyze their data trends and come to appointments with specific questions. This collaborative approach has already shown success in conditions like hypertension and Type 2 diabetes, where real-time data allows for immediate medication adjustments without the need for clinic visits [6].
In addition to fostering collaboration, RPM devices bring convenience to the forefront. Nearly half of patients (43%) cite convenience as a major benefit [6]. Features like automated reminders improve medication adherence, while continuous monitoring promotes accountability without requiring frequent trips to the doctor. The impact is clear: RPM interventions have led to better adherence to both medication and lifestyle changes [8]. Digital platforms such as Healify take it a step further by using continuous data to offer personalized coaching and actionable recommendations, deepening patient engagement in their own care journey.
5. Easier Workflows and New Revenue for Providers
Beyond saving costs and improving patient outcomes, Remote Patient Monitoring (RPM) devices are transforming how healthcare providers manage their workflows while unlocking new revenue opportunities. These FDA-cleared devices simplify processes by automatically uploading vital data - like blood pressure, glucose levels, and oxygen saturation - directly to secure cloud platforms or Electronic Health Records (EHRs) such as Epic and Oracle Cerner. Advanced RPM systems use algorithms for exception-based monitoring, flagging only abnormal readings. This allows clinical staff to focus their attention where it’s needed most, making operations more efficient and productive.
"Clinicians... need automated tools that can 'learn' from repeated exposure to vast amounts of data and surface only what's truly valuable." - Margaret Lindquist, Content Strategist, Oracle Health [4]
RPM doesn’t just streamline workflows - it generates substantial revenue for providers. Medicare RPM services allow providers to earn around $120–$150 per patient each month, adding up to over $1,000 annually per patient [6]. This revenue is tied to specific CPT codes, including:
99453: Covers initial setup and patient education.
99454: Covers monthly device supply and data transmission (requires at least 16 days of data in a 30-day period).
99457: Covers the first 20 minutes of clinical staff time for monitoring and communication.
99458: Covers each additional 20 minutes of clinical staff time [6][21].
One key advantage of RPM is that it doesn’t require direct physician involvement for routine monitoring. Under Medicare guidelines, clinical staff - like nurses or medical assistants - can handle monitoring and patient communication under general supervision [21]. This frees up physicians to focus on more complex cases, enhancing overall efficiency. Adoption of RPM by clinicians reached 81% in 2023, marking a 305% growth since 2021 [6]. Furthermore, 77% of clinicians believe RPM-enabled care will surpass traditional inpatient care within the next five years [6].
"RPM adoption from 2019 to 2022 surged ~1,300% in the U.S., a reflection of how quickly virtual care has been embraced in both chronic and acute settings." - Adrien Laurent, Content Lead [6]
To maximize benefits, providers should partner with RPM vendors that integrate seamlessly with existing systems via FHIR standards. This ensures patient data automatically populates into charts, reducing manual work. Platforms that track the 16-day data transmission requirement also help providers maintain billing compliance effortlessly. Some providers even collaborate with full-service RPM vendors offering 24/7 monitoring centers staffed by licensed nurses. These teams handle initial data reviews and escalate critical issues to physicians only when necessary. By aligning with FDA-cleared standards, these integrated platforms not only improve workflow efficiency but also enhance the broader care ecosystem.
6. Better Healthcare Access for Rural and Underserved Areas
For people living in rural areas, accessing healthcare often means long drives to the nearest clinic or hospital, which can delay necessary care. FDA-cleared remote patient monitoring (RPM) devices are changing that by bringing care directly into patients' homes. This approach removes the need for extensive travel, making both primary and specialty care more accessible. It's a game-changer for overcoming the challenges of geographic isolation.
In 2020, rural residents who utilized telemedicine and RPM were 2.01 times more likely to complete preventive care visits or services in 2021 [23]. This is a big deal because rural populations have historically struggled to access preventive healthcare due to transportation and distance issues. Additionally, tele-emergency programs in rural hospitals have proven to be cost-effective, saving approximately $3,800 per patient by avoiding unnecessary transfers to urban facilities [22].
"Telemedicine fosters a collaboration that reduces the feelings of isolation that physicians may experience when they go to practice in a small town. With telemedicine, it's like having one foot in the city but being able to live and practice out in a rural area." - Dr. Wilbur Hitt, Healthcare Provider [22]
FDA-cleared RPM devices, such as blood pressure cuffs, glucometers, pulse oximeters, and ECG patches, are bridging gaps in healthcare access. These devices automatically send accurate, medical-grade data to healthcare providers. This allows doctors to adjust medications, conduct virtual follow-ups, and step in early if readings are outside safe ranges - all without the patient needing to leave home [3][4]. By catching potential issues early, this approach helps prevent complications that could otherwise lead to emergency room visits or hospital stays, offering a vital lifeline for rural communities.
7. Personalized Care Based on Patient Data
FDA-cleared remote patient monitoring (RPM) devices are transforming healthcare by continuously collecting vital signs such as blood pressure, glucose levels, heart rhythms, and oxygen saturation. This steady flow of information offers a real-world glimpse into a patient’s health, far beyond the limited snapshot provided during a clinical visit [7]. It’s like having a window into how patients are doing in their everyday lives, not just when they’re in the doctor’s office.
The data is transmitted in real time, allowing healthcare providers to make immediate, personalized treatment decisions [3][20]. For instance, if a patient’s blood pressure stays elevated for several days, their provider can adjust medications right away instead of waiting weeks for the next appointment. These persistent trends enable providers to respond more quickly and effectively [3]. On top of that, advanced analytics take this personalization to the next level by refining treatment strategies based on the patterns revealed.
Artificial intelligence (AI) and machine learning are leading the charge in enhancing this level of care. In 2023, Biofourmis used FDA-approved algorithms to predict heart failure exacerbations before patients even noticed symptoms [6]. One health system that adopted this AI-driven RPM approach saw remarkable results: a 70% reduction in 30-day hospital readmissions and a 38% decrease in the overall cost of care [6]. AI tools also analyze continuous data to pick up early warning signs - like small changes in heart rhythm or fluid retention - that might otherwise go unnoticed [6][8].
"Digital tools are giving providers a more holistic view of patient health through access to data and giving patients more control over their health." - FDA [19]
AI-powered platforms like Healify take this personalization even further. By analyzing data from wearables, biometrics, and lifestyle factors, these tools deliver real-time, tailored health recommendations. This helps both patients and providers zero in on what truly matters, turning raw data into actionable insights. The continuous data collection enabled by RPM ensures that care is real-world and tailored to each individual’s unique needs [3].
Conclusion
FDA-cleared remote patient monitoring (RPM) devices are transforming healthcare by providing continuous, real-time data. This allows for earlier detection of potential issues, quicker treatment adjustments, and fewer hospital readmissions[4][24]. For patients, RPM devices mean fewer trips to the clinic, better management of chronic conditions, and the peace of mind that comes with consistent monitoring[4][24].
The numbers speak for themselves. Recent data shows a 19-fold increase in RPM reimbursement, signaling rapid adoption by millions of patients and healthcare providers[4][6]. This growing use of RPM technology paves the way for AI-driven advancements that promise to refine care even further.
Artificial intelligence is already adding a powerful edge to RPM. AI-guided platforms have been shown to significantly cut hospital readmissions and reduce overall care costs[6]. For example, platforms like Healify use RPM data to deliver personalized, actionable health insights, moving closer to the goal of fully tailored care.
The FDA is also playing a pivotal role in supporting this progress. Its TEMPO pilot program, launched in January 2026, highlights a commitment to driving digital health innovations aimed at improving patient outcomes[2]. Margaret Lindquist of Oracle Health captured this sentiment well:
"The World Health Organization identifies remote patient monitoring as one of a handful of healthcare delivery models with the potential to vastly improve global health outcomes"[4].
These FDA-cleared devices are laying the foundation for a new era of personalized, AI-enhanced healthcare that has the potential to improve lives on a measurable scale.
FAQs
What makes FDA-cleared remote patient monitoring (RPM) devices accurate and safe for patients?
FDA-cleared remote patient monitoring (RPM) devices focus on delivering precise measurements while ensuring patient safety. These devices are subjected to thorough validation and calibration to guarantee their sensors consistently provide dependable data. On top of that, they include strong cybersecurity features, such as encrypted data transmission and secure software, to safeguard sensitive health information.
To promote safer use, FDA guidelines emphasize proper device setup and educating patients on how to use them effectively. This approach helps users operate the devices correctly, resulting in more reliable readings and improved health management.
What financial advantages do FDA-cleared RPM devices offer for patients and healthcare providers?
Remote patient monitoring (RPM) devices that are cleared by the FDA offer a practical way for patients to cut down on healthcare expenses. By helping avoid expensive hospital stays or emergency room visits, these devices can make a real difference in managing costs.
For healthcare providers, RPM devices open the door to Medicare reimbursement opportunities while also contributing to lower overall expenses within the healthcare system.
With their focus on proactive care and early intervention, RPM devices do more than just improve health outcomes - they also ease the financial strain on patients and the system as a whole.
How do remote patient monitoring devices improve healthcare access in rural and underserved areas?
Remote patient monitoring (RPM) devices empower patients to track vital health metrics - like blood pressure, glucose levels, weight, and oxygen saturation - right from the comfort of their homes. These devices securely transmit data to healthcare providers, cutting out the need for long, often inconvenient trips to clinics. This is especially crucial in rural or underserved areas where access to healthcare providers can be limited.
Since these devices are FDA-cleared, they’re trusted for their reliability and accuracy. Medicare also supports RPM services, covering costs when patients share at least 16 readings within a 30-day period. This makes RPM a practical and affordable way to improve healthcare access, manage chronic conditions, and keep patients actively involved in their health.
Healify takes RPM a step further by combining it with AI-powered health coaching. Its virtual coach is available 24/7, offering personalized advice and real-time support. For patients in remote areas, this means staying on top of their health and receiving guidance, even without frequent in-person visits to a doctor’s office.
Related Blog Posts
Endlich die Kontrolle über Ihre Gesundheit übernehmen

Endlich die Kontrolle über Ihre Gesundheit übernehmen

Endlich die Kontrolle über Ihre Gesundheit übernehmen





