Improve your health
Improve your health
Improve your health
11. Dezember 2025
How AI Enhances Wearable Post-Surgery Monitoring


Recovering from surgery is a critical phase where complications like infections, blood clots, or irregular heart rhythms can arise. Traditional monitoring often misses early warning signs due to periodic checks. AI-powered wearables - like smartwatches, patches, and biosensors - are transforming this process by offering continuous tracking of vital signs such as heart rate, oxygen levels, temperature, and movement.
Key benefits include:
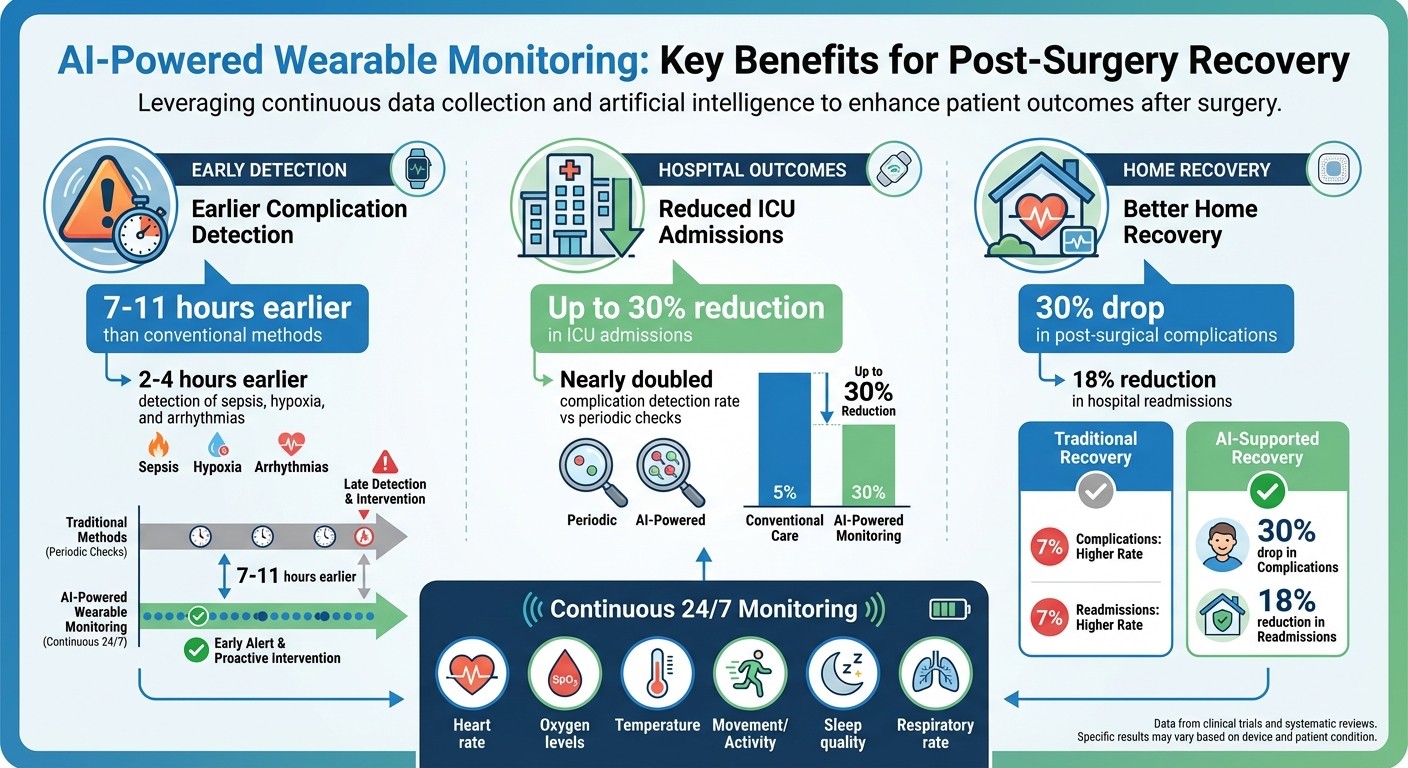
Early Detection: AI identifies complications 7–11 hours earlier than conventional methods, reducing ICU admissions by up to 30%.
Shorter Hospital Stays: Continuous monitoring leads to fewer readmissions and quicker recoveries.
Personalized Recovery Plans: AI tailors goals based on surgery type, health data, and patient progress.
Home Monitoring: Patients recover safely at home with 24/7 oversight and alerts for concerning trends.
Apps like Healify simplify recovery by combining wearable data with actionable insights. For example, it tracks mobility, sleep, and stress while offering daily recommendations like walking goals or relaxation techniques. AI-driven alerts ensure timely medical interventions, making recovery safer and more effective.
These advancements are reshaping post-surgical care by prioritizing patient safety and personalized recovery.
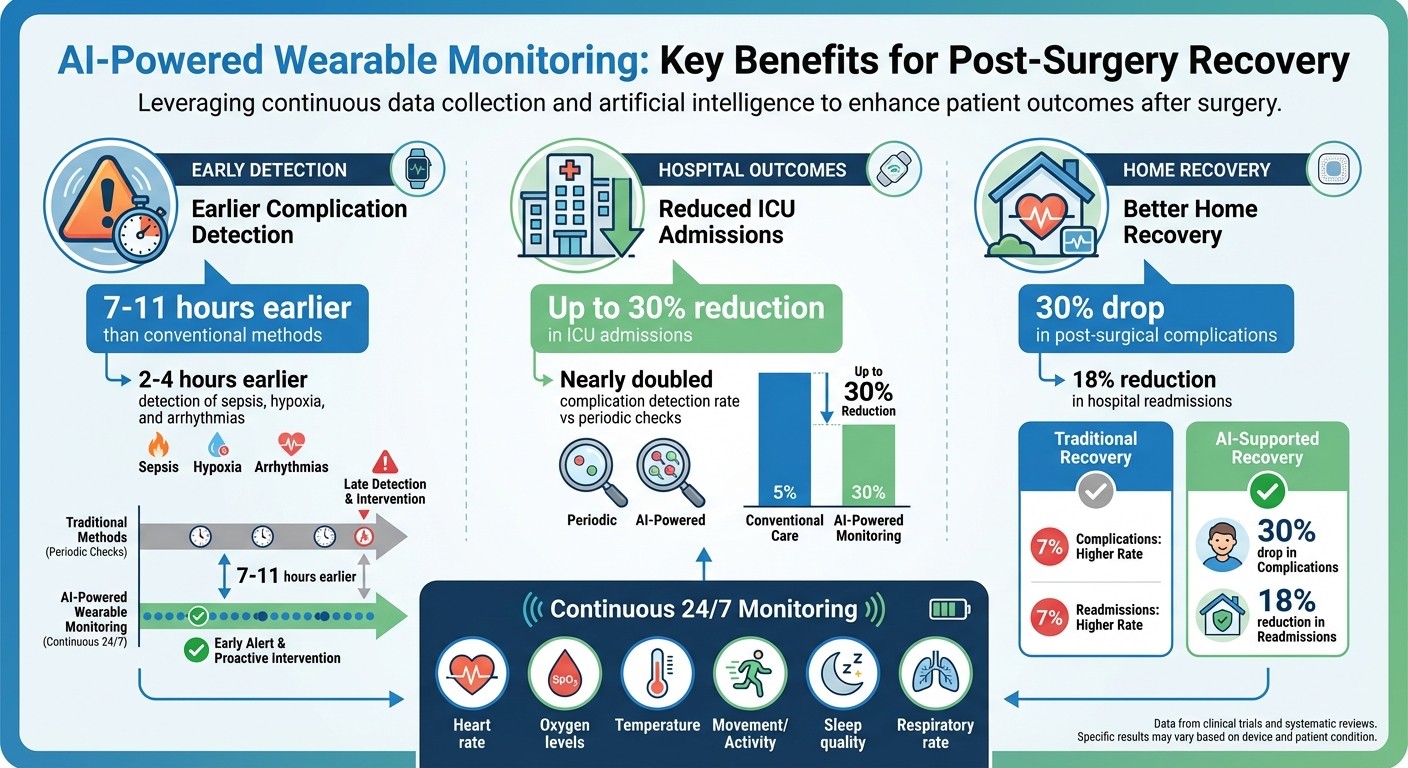
AI-Powered Wearable Monitoring: Key Benefits and Statistics for Post-Surgery Recovery
Understanding Post-Surgery Monitoring and Wearable Devices
Why Post-Surgery Monitoring Matters
After surgery, patients are at risk for complications like infections, deep vein thrombosis, respiratory issues, sepsis, arrhythmias, and bleeding. These problems can lead to longer hospital stays and more ICU admissions [2][6].
Traditional monitoring methods, which rely on periodic checks, can sometimes miss subtle warning signs. For instance, a slight increase in heart rate, a drop in oxygen levels, or a rise in temperature might go unnoticed until the problem becomes more serious [2][3].
How Wearables Are Used in Post-Surgery Care
Wearable devices play a critical role in bridging these gaps by providing continuous tracking of vital signs. Patch-style sensors, worn on the chest or upper arm, monitor key metrics like heart rate, respiratory rate, oxygen saturation (SpO₂), skin temperature, and movement. Meanwhile, wrist-worn devices, such as smartwatches, use photoplethysmography (PPG) to measure heart rate and activity levels, while accelerometers track sleep and mobility [2][3].
These devices are used in multiple settings, starting in the hospital recovery unit, continuing on the ward, and even at home after discharge. Specialized wearables, like smart rings, ankle bands, and bandages, can detect wound temperature and moisture changes - potential early signs of infection. For patients recovering from orthopedic procedures, devices that monitor gait and limb movement provide objective data on their rehabilitation progress [3][8].
By continuously collecting this data, wearables create a foundation for AI to analyze patient-specific trends and enable timely medical interventions.
How AI Improves Wearable Performance
Continuous monitoring generates a massive amount of data, which can be overwhelming for healthcare teams. This is where AI steps in, transforming raw data into meaningful insights. AI algorithms filter out irrelevant information caused by movement or sensor shifts and focus on identifying significant patterns over time [3][6].
AI doesn’t just flag every minor fluctuation. Instead, it learns each patient’s baseline - covering metrics like heart rate, mobility, and sleep patterns - and identifies persistent changes that may signal a problem [6][8]. This capability ensures that data isn’t just collected but actively used to drive timely clinical decisions, moving post-surgical care toward a more proactive approach.
Clinical trials have shown that AI-powered systems can detect complications like hypoxia, sepsis, and arrhythmias 2 to 4 hours earlier than traditional methods. These advancements have been associated with up to a 30% reduction in ICU admissions for surgical patients [6][10]. When risk thresholds are exceeded, automated alerts appear on clinician dashboards, prompting immediate bedside evaluations and interventions [2][4].
Main Benefits of AI-Powered Wearable Monitoring
Catching Complications Early
AI-powered wearables are proving to be a game-changer when it comes to spotting complications before they escalate. By analyzing key metrics like heart rate, respiratory rate, oxygen saturation, and temperature, AI systems can detect sepsis 2–4 hours earlier than traditional methods. This extra time can be critical for initiating treatment and potentially saving lives [10]. What’s impressive is how these devices adapt to each patient by learning their baseline readings across multiple health parameters. When persistent deviations occur, the system flags potential issues such as infections or bleeding [6]. Research shows that these early warnings can lead to shorter hospital stays, fewer ICU transfers, and a drop in readmission rates [2].
But the benefits don’t stop at early detection. AI also plays a pivotal role in shaping recovery plans that are tailored to each individual.
Custom Recovery Plans for Each Patient
AI takes the guesswork out of recovery by crafting personalized plans based on a combination of factors - surgery type, preoperative fitness, age, comorbidities, and real-time wearable data. For example, after a joint replacement, algorithms analyze your step count, range of motion, and sleep patterns. Then, they compare your progress to benchmarks from similar patients, adjusting your walking goals and physical therapy exercises accordingly [11].
In trials for cardiac and thoracic surgeries, patients using wearables with structured feedback reported remarkable improvements. They increased physical activity in the first few weeks post-op and experienced better physical function, lower pain levels at two weeks, and even less shortness of breath at both two weeks and six months compared to those receiving standard care [7]. Platforms like Healify go a step further by combining wearable data with biometrics, bloodwork, and lifestyle habits. This integration allows for 24/7 AI-driven coaching, offering simple, actionable advice - like setting walking targets, practicing breathing exercises, or improving sleep routines (https://healify.ai) [1].
Instant Alerts and Clinical Support
One of the standout features of AI-powered wearables is their ability to provide instant alerts. If the system detects concerning patterns - like a sustained drop in oxygen levels or a rapid heart rate paired with fever - it sends immediate notifications to both the patient and their care team. This triggers timely interventions, whether it’s a bedside assessment, lab orders, or adjustments to treatment plans in hospitals, or remote reviews by nurses and surgeons for those recovering at home [2][11].
This layered alert system has shown real-world benefits, including a 30% reduction in ICU admissions when AI-driven analytics are used for postoperative monitoring [10]. The technology ensures that only the most critical events are prioritized, escalating from app-based coaching to telehealth consultations or urgent care recommendations based on severity [11]. By offering continuous oversight, these systems make earlier discharges safer and help patients feel more confident recovering in the comfort of their own homes [2].
Real-World Uses: AI in Post-Surgery Recovery
Monitoring Patients in the Hospital
Hospitals across the United States are equipping high-risk surgical patients with patch-style sensors on their chests and wrist-worn devices immediately after major surgeries. These wearables continuously monitor vital signs like heart rate, respiratory rate, oxygen saturation (SpO₂), skin temperature, and movement, streaming the data in real time to care teams [2][6]. Unlike traditional checks done every few hours, AI algorithms process this constant flow of information, identifying subtle changes that could indicate potential issues.
The impact has been striking. Continuous monitoring with wearables has nearly doubled the rate of complication detection compared to periodic checks. This allows care teams to intervene earlier, leading to shorter hospital stays, fewer ICU transfers, and reduced readmissions [2]. For instance, if a patient’s respiratory rate gradually rises while oxygen levels drop, the system sends alerts to the care team through dashboards, pagers, or mobile apps. Nurses can then assess the patient in person, and doctors can order necessary tests or treatments before the situation escalates [2][4].
This approach has been particularly effective for patients recovering from major surgeries like abdominal, cardiac, or thoracic procedures. Systems such as SensiumVitals, HealthPatch, and Masimo Radius-7 have shown that changes in vital signs often occur 5 to 11 hours before patients exhibit noticeable symptoms of deterioration [2]. Some hospitals have even reported up to a 30% reduction in ICU admissions when AI-driven monitoring is part of postoperative care for high-risk patients [10].
These benefits don’t end at the hospital doors - AI-powered monitoring continues to play a critical role during home recovery.
Supporting Recovery at Home
After leaving the hospital, patients can rely on AI-integrated wearables to support their recovery at home. Devices like smartwatches and patches track metrics such as step count, heart rate, oxygen saturation, skin temperature, and sleep quality [3][5][12]. This data feeds into remote monitoring systems, where AI models look for deviations from a patient’s normal range - like a sudden decrease in daily steps or a rise in heart rate and skin temperature, which could indicate an infection or blood clot.
These programs have delivered measurable results. Some studies show a 30% drop in post-surgical complications thanks to early detection of warning signs, while one initiative documented an 18% reduction in hospital readmissions for surgical patients [3]. When concerning patterns emerge, care teams can act quickly through telehealth consultations, medication adjustments, remote wound checks, or early in-person evaluations - often preventing emergency room visits.
For example, patients recovering from abdominal surgery have used smart patches to detect subtle increases in skin temperature and heart rate variability 24 to 48 hours before visible signs of infection appear. This early detection allows for timely antibiotic treatment, often avoiding the need for additional surgery [3][2]. Similarly, cardiac surgery patients have benefited from continuous monitoring, with AI identifying early signs of atrial fibrillation or heart failure, enabling prompt medication adjustments [6][12].
Tracking Pain, Sleep, and Stress Levels
AI doesn’t just monitor physical recovery - it also helps manage pain, sleep, and stress. By analyzing data like elevated resting heart rate, increased respiratory rate, reduced activity levels, disrupted sleep, and heart rate variability, AI models can estimate pain levels and suggest changes to medication schedules or non-drug interventions like breathing exercises [3][5][10].
Sleep tracking is another area where wearables shine. Using accelerometry and heart rate patterns, they provide insights into sleep duration, efficiency, nighttime awakenings, and timing [3][5]. In hospitals, this data helps identify patients whose recovery is hindered by poor sleep, prompting adjustments to nighttime routines or medications [6][8]. At home, AI systems monitor sleep improvements over time and recommend strategies like earlier bedtimes or relaxation techniques when needed. Better sleep often correlates with improved pain management and faster recovery [3][5].
Stress levels, too, are monitored through metrics like low heart rate variability and elevated resting heart rate over several days [3][5][12]. AI can flag these patterns and suggest interventions such as guided breathing exercises, mindfulness activities, or reduced activity intensity. These tools add another layer of support, addressing the emotional and physiological challenges of recovery.
Platforms like Healify combine wearable data with lifestyle and biometric insights to provide round-the-clock AI-guided coaching. Through its virtual assistant, Anna, the app offers actionable advice - like setting walking goals, practicing relaxation techniques, or improving sleep habits. If the data suggests clinical issues like anxiety, depression, or physiological instability, the system can escalate the case to a healthcare provider (https://healify.ai) [1].
How Healify Supports Post-Surgery Monitoring
How Healify Makes Recovery Easier
Healify simplifies the often overwhelming process of post-surgery recovery by turning complex data into clear, actionable guidance.
After surgery, wearables generate a flood of data that can be hard to interpret. Healify takes all those numbers and boils them down into a single, easy-to-understand health score ranging from 0 to 100. This score quickly shows whether you're on track, slightly off, or in need of attention. Instead of sifting through raw metrics, you get straightforward updates like, "Today's recovery is on track" or "Slightly off track - main issue: low mobility", paired with intuitive color codes and trend indicators.
The app goes a step further by creating personalized recovery milestones tailored to your surgery type, age, fitness level, and your surgeon's recommendations. It then translates these milestones into specific daily tasks. For instance, if you've had knee replacement surgery, your goals for the first week might include "Walk 5–10 minutes every hour while awake" or "Reach 2,000–2,500 steps today." If your progress deviates, Healify adjusts your plan with actionable steps like, "Sleep 20 minutes earlier and take a 10-minute walk to boost activity." As you achieve these milestones, the app gradually increases your goals in manageable increments, ensuring steady progress without overexertion.
This approach is particularly helpful during recovery when you might feel fatigued, in pain, or overwhelmed by medications. By breaking down complex data into just 1–3 clear recommendations per day, Healify ensures you stay focused on what matters most without feeling overloaded.
Features Designed for Post-Surgery Patients
Healify extends its monitoring capabilities into personalized, proactive recovery strategies designed specifically for post-surgery patients.
Anna, Healify's 24/7 AI health coach, uses real-time wearable data and your feedback to address common recovery challenges like pain and mobility. For example, if you report that your pain has increased from 4/10 to 7/10 after walking, and your wearable shows no alarming changes in heart rate or oxygen levels, Anna might suggest: "This level of soreness is normal after increasing activity. Let's reduce today's steps by 20% and add an ice-and-rest routine: 15 minutes of ice followed by 45 minutes without, repeated three times." If your wearable shows a rising nighttime heart rate and decreased deep sleep, Anna could recommend strategies like taking pain medication earlier in the evening, a 10-minute breathing exercise, and avoiding screens an hour before bed.
For sleep, Healify merges wearable data with your input to pinpoint issues like "pain spikes at 2:00 a.m." and offers solutions such as relaxation techniques, timing adjustments, and environmental changes to help you achieve 7–9 hours of rest. For stress, it tracks heart rate variability and breathing patterns, suggesting quick interventions like guided breathing exercises, short walks, or reframing techniques when stress levels rise. For mobility, the app analyzes step counts, sit-stand frequency, and gait smoothness to create activity goals that align with your surgeon's limits. These might include "Stand up once every hour" or "Reach 3,000 steps by the end of week two", with adjustments based on your pain, fatigue, and progress.
Healify also provides smart alerts when sustained changes in your data suggest potential complications. For instance, if your resting heart rate rises, daily step count drops over several days, oxygen levels decrease, or nighttime temperature steadily increases, the app might notify you: "Your heart rate and skin temperature have been elevated for 24 hours, and your activity is down. This could indicate a problem. Contact your surgeon's office or visit urgent care if your symptoms worsen." These alerts are designed to catch issues early without overwhelming you with unnecessary notifications, ensuring peace of mind as you recover at home.
Challenges of AI-Powered Monitoring Systems
Technical and Clinical Limitations
AI-driven wearables often face hurdles in accuracy due to motion artifacts and poor sensor contact, which can lead to false alarms. Issues like limited battery life and unreliable connectivity can further disrupt the timely transmission of critical data.
On the clinical side, validation remains a challenge. For instance, a systematic review of wearables used after abdominal surgery revealed significant variations in devices, metrics, and study methods. The review concluded there is "insufficient high‑quality evidence to support routine clinical use" [9]. Many algorithms are trained on small, single-center datasets, which can limit their effectiveness in broader, more diverse settings. This often forces clinicians to double-check wearable data with bedside measurements or even disregard alerts when confidence in the system wanes.
False positives can overwhelm nursing staff with unnecessary alerts, while false negatives might miss critical signs of complications like sepsis, bleeding, or respiratory failure. To address these issues, hospitals can adjust alert thresholds and implement tiered notifications to reduce alarm fatigue. However, these solutions require continuous fine-tuning and staff training to be effective.
Privacy and Data Security Issues
Beyond technical challenges, protecting patient data adds another layer of complexity.
Continuous monitoring generates a steady stream of sensitive information - such as vital signs, sleep patterns, mobility, and even location - that offers detailed insights into a patient’s health. As this data moves between hospital systems, cloud platforms, consumer wearables, and mobile apps, it passes through multiple hands, including device manufacturers, cloud providers, analytics companies, and app developers. This increases the risk of unauthorized access or misuse.
In the United States, HIPAA requires healthcare organizations and their partners to safeguard protected health information by encrypting data, enforcing strict access controls, and maintaining detailed access logs. However, weak security measures - like poor authentication protocols or unclear data-sharing practices - can lead to compliance issues and put patient privacy at risk. To mitigate these risks, hospitals must establish strong vendor agreements, conduct regular security audits, and maintain clear incident-response plans.
Access and Affordability Barriers
Economic and infrastructure challenges also limit the widespread use of AI-powered monitoring systems.
The upfront cost of hardware, such as patches, smartwatches, and sensors, can range from tens to hundreds of dollars per patient, depending on whether the devices are disposable or reusable. Recurring expenses for software licenses, cloud hosting, EHR integration, technical support, staff training, and workflow adjustments add to the financial strain. Without clear reimbursement policies from Medicare, Medicaid, or private insurers, hospitals may hesitate to invest in these technologies, leaving patients to shoulder potential out-of-pocket expenses.
Reliable infrastructure is another critical factor. Real-time data uploads require consistent broadband or cellular coverage, yet rural areas and some urban, low-income neighborhoods often lack reliable connectivity. Patients also need compatible smartphones - like an iPhone for syncing with certain wearables such as Healify - which creates an additional barrier for those without the necessary devices. Older adults, individuals with cognitive impairments, or those with limited digital literacy may struggle with tasks like charging devices, wearing them correctly, or troubleshooting connectivity issues. These challenges can lead to poor data quality or early abandonment of the technology. Language barriers and poorly designed interfaces that don’t align with diverse user needs further reduce engagement among minority populations, deepening the digital divide. As a result, patients with better resources gain access to advanced monitoring, while others are left with traditional, less frequent follow-ups.
Addressing these obstacles is crucial to unlocking the full potential of AI in improving post-surgical care and recovery outcomes.
What's Next for AI in Post-Surgery Monitoring
Moving from Monitoring to Prediction
AI is steadily evolving from a tool for reactive monitoring to one that can proactively predict complications before they become severe. This shift could redefine how post-surgery care is managed.
Future AI-driven wearables are expected to predict complications hours before they show obvious clinical signs. These systems will adapt to each patient by learning their unique baseline metrics and considering factors like the type of surgery, medications, and existing health conditions [6].
Studies suggest that AI systems can detect complications earlier than traditional monitoring methods, which could lead to fewer ICU transfers, shorter hospital stays, and reduced readmissions [2]. In the U.S., these tools are likely to integrate seamlessly with early warning systems and electronic health records (EHRs), enabling care teams to act based on risk forecasts rather than waiting for emergencies to arise.
Some of the primary areas where AI could make a difference include identifying infections and sepsis by analyzing subtle changes in temperature, heart rate, and variability. It could also predict cardiorespiratory issues such as arrhythmias and hypoxia, thromboembolic events linked to immobility, and even pain flares that could slow recovery [6]. AI platforms are already being used to identify patients at high risk for acute kidney injury, guiding targeted interventions [5]. These advancements could help tailor discharge plans, follow-up schedules, and home care support to each patient’s specific needs.
New Technologies on the Horizon
The next wave of innovation is set to go beyond the familiar smartwatches and chest patches, bringing monitoring closer to the surgical site itself. For instance, smart wound dressings equipped with sensors will monitor local factors like temperature, pH levels, moisture, and biochemical markers. These dressings could even release medication automatically if they detect an infection or other complications [3].
Implantable sensors are another exciting development. Orthopedic and cardiac devices embedded with strain, pressure, or motion sensors could keep tabs on implant stability, detect early signs of failure, and track rehabilitation progress. These sensors would allow AI systems to differentiate between normal recovery and potential problems [5]. Additionally, advanced multi-sensor patches and smart textiles are being developed to continuously measure vital signs, feeding real-time data into recovery and risk assessments [6].
These technologies will likely integrate with consumer devices like the Apple Watch and Fitbit. AI platforms will act as the central hub, synthesizing data from clinical-grade patches, smart dressings, and consumer wearables into streamlined dashboards for healthcare providers. On the patient side, apps like Healify are already combining wearable, biometric, and lifestyle data to offer 24/7 personalized recovery guidance. These apps can provide actionable advice - such as setting daily walking goals, sending wound-care reminders, or suggesting breathing exercises - and issue alerts when concerning trends appear [4]. Such tools are paving the way for broader adoption in clinical practice.
Research and Implementation Needs
For these advancements to become a routine part of postoperative care, rigorous research and thoughtful implementation strategies are essential. Large-scale, multicenter trials across diverse U.S. hospitals will be needed to confirm that AI-enhanced devices actually reduce complications, hospital stays, ICU transfers, and mortality rates [10]. Predictive models must also undergo external validation, including subgroup analyses that account for factors like age, race, ethnicity, socioeconomic status, and preexisting conditions to minimize bias [4].
Cost-effectiveness will also play a critical role. Studies must weigh the expenses of devices, data infrastructure, and staffing against the potential savings from fewer complications and reduced hospital utilization [2]. Additionally, human factors like patient adherence, device comfort, alarm fatigue, and clinician workload must be addressed to ensure these technologies are practical and effective.
Hospitals will need clear protocols to determine which patients should use these devices and for how long - such as 7 to 30 days post-discharge. Thresholds for triggering interventions, whether through nursing calls, telehealth appointments, or in-person evaluations, should be well-defined. Establishing dedicated remote monitoring teams, such as telemetry nurses or advanced practice providers, will be crucial for managing AI alerts and coordinating follow-up care. By integrating these predictive systems into existing EHR workflows and focusing on proactive monitoring rather than adding more alarms, healthcare systems can significantly improve patient recovery and streamline postoperative care. This shift toward predictive, data-driven care has the potential to transform the way hospitals approach recovery and risk management.
Is This the Future of Patient Care? Remote Patient Monitoring, Wearables & AI
Conclusion: Better Recovery Through AI Wearables
AI-powered wearables are revolutionizing post-surgery care by offering continuous, real-time monitoring that catches complications early and tailors recovery plans to each patient. These devices track vital metrics like heart rate, oxygen levels, temperature, mobility, sleep, and pain, ensuring a personalized approach to recovery. Studies have shown that this level of early detection leads to better outcomes for patients.
By analyzing a patient’s baseline data, AI can fine-tune recovery goals - adjusting activity levels, rest periods, and alert thresholds based on factors like age, type of surgery, and overall health. This means patients receive specific, actionable recommendations that help them rebuild strength and confidence during their recovery journey.
For patients recovering at home in the U.S., Healify makes this cutting-edge technology accessible and easy to use. It connects seamlessly with Apple-compatible wearables, analyzing vital signs, activity patterns, sleep quality, and stress levels. The app then translates this data into simple daily tasks, such as "Take 3,000 steps today in smaller intervals" or "Your sleep has been under 6 hours for three nights - here’s how to improve it." Healify’s 24/7 AI health coach, Anna, provides clear recovery guidance, flags potential issues, and prompts users to reach out to their care team when necessary. By combining precise data tracking with actionable insights, Healify demonstrates how technology is transforming post-surgery care into a safer, more personalized experience.
FAQs
How can AI wearables help detect post-surgery complications earlier?
AI-powered wearables bring a new level of convenience and precision to health monitoring by tracking vital signs, stress levels, and other important health metrics in real time. They don’t just collect data - they analyze it to spot subtle changes, like an irregular heartbeat or a spike in stress hormones, long before symptoms become apparent.
This ability to catch early warning signs means quicker intervention, potentially stopping small issues from turning into major health concerns. These devices do more than just inform - they enable patients and healthcare providers to make timely, well-informed decisions that can significantly impact recovery.
What kind of data do AI-powered wearables collect to tailor recovery plans?
AI-powered wearables collect a wide range of health data to design recovery plans tailored to individual needs. They track activity levels, sleep quality, stress markers, hydration levels, and biometric details like heart rate and cortisol levels.
With this data, these devices provide real-time insights and practical feedback, helping users improve recovery and enhance their overall well-being.
What challenges come with using AI-powered wearables for post-surgery monitoring?
Implementing AI-powered wearables in post-surgery care comes with its own set of hurdles. Data privacy tops the list, as handling sensitive health information requires airtight security measures. On top of that, integrating these devices into current healthcare systems can be a tricky and time-intensive process.
Another critical factor is ensuring the accuracy and reliability of the AI algorithms. False alarms or overlooked issues could compromise patient safety and trust. Speaking of trust, patient acceptance of these technologies is essential for their widespread adoption. Lastly, effectively managing the flood of real-time data these devices generate - without overwhelming healthcare teams or patients - is a challenge that cannot be ignored.
Related Blog Posts
Recovering from surgery is a critical phase where complications like infections, blood clots, or irregular heart rhythms can arise. Traditional monitoring often misses early warning signs due to periodic checks. AI-powered wearables - like smartwatches, patches, and biosensors - are transforming this process by offering continuous tracking of vital signs such as heart rate, oxygen levels, temperature, and movement.
Key benefits include:
Early Detection: AI identifies complications 7–11 hours earlier than conventional methods, reducing ICU admissions by up to 30%.
Shorter Hospital Stays: Continuous monitoring leads to fewer readmissions and quicker recoveries.
Personalized Recovery Plans: AI tailors goals based on surgery type, health data, and patient progress.
Home Monitoring: Patients recover safely at home with 24/7 oversight and alerts for concerning trends.
Apps like Healify simplify recovery by combining wearable data with actionable insights. For example, it tracks mobility, sleep, and stress while offering daily recommendations like walking goals or relaxation techniques. AI-driven alerts ensure timely medical interventions, making recovery safer and more effective.
These advancements are reshaping post-surgical care by prioritizing patient safety and personalized recovery.
AI-Powered Wearable Monitoring: Key Benefits and Statistics for Post-Surgery Recovery
Understanding Post-Surgery Monitoring and Wearable Devices
Why Post-Surgery Monitoring Matters
After surgery, patients are at risk for complications like infections, deep vein thrombosis, respiratory issues, sepsis, arrhythmias, and bleeding. These problems can lead to longer hospital stays and more ICU admissions [2][6].
Traditional monitoring methods, which rely on periodic checks, can sometimes miss subtle warning signs. For instance, a slight increase in heart rate, a drop in oxygen levels, or a rise in temperature might go unnoticed until the problem becomes more serious [2][3].
How Wearables Are Used in Post-Surgery Care
Wearable devices play a critical role in bridging these gaps by providing continuous tracking of vital signs. Patch-style sensors, worn on the chest or upper arm, monitor key metrics like heart rate, respiratory rate, oxygen saturation (SpO₂), skin temperature, and movement. Meanwhile, wrist-worn devices, such as smartwatches, use photoplethysmography (PPG) to measure heart rate and activity levels, while accelerometers track sleep and mobility [2][3].
These devices are used in multiple settings, starting in the hospital recovery unit, continuing on the ward, and even at home after discharge. Specialized wearables, like smart rings, ankle bands, and bandages, can detect wound temperature and moisture changes - potential early signs of infection. For patients recovering from orthopedic procedures, devices that monitor gait and limb movement provide objective data on their rehabilitation progress [3][8].
By continuously collecting this data, wearables create a foundation for AI to analyze patient-specific trends and enable timely medical interventions.
How AI Improves Wearable Performance
Continuous monitoring generates a massive amount of data, which can be overwhelming for healthcare teams. This is where AI steps in, transforming raw data into meaningful insights. AI algorithms filter out irrelevant information caused by movement or sensor shifts and focus on identifying significant patterns over time [3][6].
AI doesn’t just flag every minor fluctuation. Instead, it learns each patient’s baseline - covering metrics like heart rate, mobility, and sleep patterns - and identifies persistent changes that may signal a problem [6][8]. This capability ensures that data isn’t just collected but actively used to drive timely clinical decisions, moving post-surgical care toward a more proactive approach.
Clinical trials have shown that AI-powered systems can detect complications like hypoxia, sepsis, and arrhythmias 2 to 4 hours earlier than traditional methods. These advancements have been associated with up to a 30% reduction in ICU admissions for surgical patients [6][10]. When risk thresholds are exceeded, automated alerts appear on clinician dashboards, prompting immediate bedside evaluations and interventions [2][4].
Main Benefits of AI-Powered Wearable Monitoring
Catching Complications Early
AI-powered wearables are proving to be a game-changer when it comes to spotting complications before they escalate. By analyzing key metrics like heart rate, respiratory rate, oxygen saturation, and temperature, AI systems can detect sepsis 2–4 hours earlier than traditional methods. This extra time can be critical for initiating treatment and potentially saving lives [10]. What’s impressive is how these devices adapt to each patient by learning their baseline readings across multiple health parameters. When persistent deviations occur, the system flags potential issues such as infections or bleeding [6]. Research shows that these early warnings can lead to shorter hospital stays, fewer ICU transfers, and a drop in readmission rates [2].
But the benefits don’t stop at early detection. AI also plays a pivotal role in shaping recovery plans that are tailored to each individual.
Custom Recovery Plans for Each Patient
AI takes the guesswork out of recovery by crafting personalized plans based on a combination of factors - surgery type, preoperative fitness, age, comorbidities, and real-time wearable data. For example, after a joint replacement, algorithms analyze your step count, range of motion, and sleep patterns. Then, they compare your progress to benchmarks from similar patients, adjusting your walking goals and physical therapy exercises accordingly [11].
In trials for cardiac and thoracic surgeries, patients using wearables with structured feedback reported remarkable improvements. They increased physical activity in the first few weeks post-op and experienced better physical function, lower pain levels at two weeks, and even less shortness of breath at both two weeks and six months compared to those receiving standard care [7]. Platforms like Healify go a step further by combining wearable data with biometrics, bloodwork, and lifestyle habits. This integration allows for 24/7 AI-driven coaching, offering simple, actionable advice - like setting walking targets, practicing breathing exercises, or improving sleep routines (https://healify.ai) [1].
Instant Alerts and Clinical Support
One of the standout features of AI-powered wearables is their ability to provide instant alerts. If the system detects concerning patterns - like a sustained drop in oxygen levels or a rapid heart rate paired with fever - it sends immediate notifications to both the patient and their care team. This triggers timely interventions, whether it’s a bedside assessment, lab orders, or adjustments to treatment plans in hospitals, or remote reviews by nurses and surgeons for those recovering at home [2][11].
This layered alert system has shown real-world benefits, including a 30% reduction in ICU admissions when AI-driven analytics are used for postoperative monitoring [10]. The technology ensures that only the most critical events are prioritized, escalating from app-based coaching to telehealth consultations or urgent care recommendations based on severity [11]. By offering continuous oversight, these systems make earlier discharges safer and help patients feel more confident recovering in the comfort of their own homes [2].
Real-World Uses: AI in Post-Surgery Recovery
Monitoring Patients in the Hospital
Hospitals across the United States are equipping high-risk surgical patients with patch-style sensors on their chests and wrist-worn devices immediately after major surgeries. These wearables continuously monitor vital signs like heart rate, respiratory rate, oxygen saturation (SpO₂), skin temperature, and movement, streaming the data in real time to care teams [2][6]. Unlike traditional checks done every few hours, AI algorithms process this constant flow of information, identifying subtle changes that could indicate potential issues.
The impact has been striking. Continuous monitoring with wearables has nearly doubled the rate of complication detection compared to periodic checks. This allows care teams to intervene earlier, leading to shorter hospital stays, fewer ICU transfers, and reduced readmissions [2]. For instance, if a patient’s respiratory rate gradually rises while oxygen levels drop, the system sends alerts to the care team through dashboards, pagers, or mobile apps. Nurses can then assess the patient in person, and doctors can order necessary tests or treatments before the situation escalates [2][4].
This approach has been particularly effective for patients recovering from major surgeries like abdominal, cardiac, or thoracic procedures. Systems such as SensiumVitals, HealthPatch, and Masimo Radius-7 have shown that changes in vital signs often occur 5 to 11 hours before patients exhibit noticeable symptoms of deterioration [2]. Some hospitals have even reported up to a 30% reduction in ICU admissions when AI-driven monitoring is part of postoperative care for high-risk patients [10].
These benefits don’t end at the hospital doors - AI-powered monitoring continues to play a critical role during home recovery.
Supporting Recovery at Home
After leaving the hospital, patients can rely on AI-integrated wearables to support their recovery at home. Devices like smartwatches and patches track metrics such as step count, heart rate, oxygen saturation, skin temperature, and sleep quality [3][5][12]. This data feeds into remote monitoring systems, where AI models look for deviations from a patient’s normal range - like a sudden decrease in daily steps or a rise in heart rate and skin temperature, which could indicate an infection or blood clot.
These programs have delivered measurable results. Some studies show a 30% drop in post-surgical complications thanks to early detection of warning signs, while one initiative documented an 18% reduction in hospital readmissions for surgical patients [3]. When concerning patterns emerge, care teams can act quickly through telehealth consultations, medication adjustments, remote wound checks, or early in-person evaluations - often preventing emergency room visits.
For example, patients recovering from abdominal surgery have used smart patches to detect subtle increases in skin temperature and heart rate variability 24 to 48 hours before visible signs of infection appear. This early detection allows for timely antibiotic treatment, often avoiding the need for additional surgery [3][2]. Similarly, cardiac surgery patients have benefited from continuous monitoring, with AI identifying early signs of atrial fibrillation or heart failure, enabling prompt medication adjustments [6][12].
Tracking Pain, Sleep, and Stress Levels
AI doesn’t just monitor physical recovery - it also helps manage pain, sleep, and stress. By analyzing data like elevated resting heart rate, increased respiratory rate, reduced activity levels, disrupted sleep, and heart rate variability, AI models can estimate pain levels and suggest changes to medication schedules or non-drug interventions like breathing exercises [3][5][10].
Sleep tracking is another area where wearables shine. Using accelerometry and heart rate patterns, they provide insights into sleep duration, efficiency, nighttime awakenings, and timing [3][5]. In hospitals, this data helps identify patients whose recovery is hindered by poor sleep, prompting adjustments to nighttime routines or medications [6][8]. At home, AI systems monitor sleep improvements over time and recommend strategies like earlier bedtimes or relaxation techniques when needed. Better sleep often correlates with improved pain management and faster recovery [3][5].
Stress levels, too, are monitored through metrics like low heart rate variability and elevated resting heart rate over several days [3][5][12]. AI can flag these patterns and suggest interventions such as guided breathing exercises, mindfulness activities, or reduced activity intensity. These tools add another layer of support, addressing the emotional and physiological challenges of recovery.
Platforms like Healify combine wearable data with lifestyle and biometric insights to provide round-the-clock AI-guided coaching. Through its virtual assistant, Anna, the app offers actionable advice - like setting walking goals, practicing relaxation techniques, or improving sleep habits. If the data suggests clinical issues like anxiety, depression, or physiological instability, the system can escalate the case to a healthcare provider (https://healify.ai) [1].
How Healify Supports Post-Surgery Monitoring
How Healify Makes Recovery Easier
Healify simplifies the often overwhelming process of post-surgery recovery by turning complex data into clear, actionable guidance.
After surgery, wearables generate a flood of data that can be hard to interpret. Healify takes all those numbers and boils them down into a single, easy-to-understand health score ranging from 0 to 100. This score quickly shows whether you're on track, slightly off, or in need of attention. Instead of sifting through raw metrics, you get straightforward updates like, "Today's recovery is on track" or "Slightly off track - main issue: low mobility", paired with intuitive color codes and trend indicators.
The app goes a step further by creating personalized recovery milestones tailored to your surgery type, age, fitness level, and your surgeon's recommendations. It then translates these milestones into specific daily tasks. For instance, if you've had knee replacement surgery, your goals for the first week might include "Walk 5–10 minutes every hour while awake" or "Reach 2,000–2,500 steps today." If your progress deviates, Healify adjusts your plan with actionable steps like, "Sleep 20 minutes earlier and take a 10-minute walk to boost activity." As you achieve these milestones, the app gradually increases your goals in manageable increments, ensuring steady progress without overexertion.
This approach is particularly helpful during recovery when you might feel fatigued, in pain, or overwhelmed by medications. By breaking down complex data into just 1–3 clear recommendations per day, Healify ensures you stay focused on what matters most without feeling overloaded.
Features Designed for Post-Surgery Patients
Healify extends its monitoring capabilities into personalized, proactive recovery strategies designed specifically for post-surgery patients.
Anna, Healify's 24/7 AI health coach, uses real-time wearable data and your feedback to address common recovery challenges like pain and mobility. For example, if you report that your pain has increased from 4/10 to 7/10 after walking, and your wearable shows no alarming changes in heart rate or oxygen levels, Anna might suggest: "This level of soreness is normal after increasing activity. Let's reduce today's steps by 20% and add an ice-and-rest routine: 15 minutes of ice followed by 45 minutes without, repeated three times." If your wearable shows a rising nighttime heart rate and decreased deep sleep, Anna could recommend strategies like taking pain medication earlier in the evening, a 10-minute breathing exercise, and avoiding screens an hour before bed.
For sleep, Healify merges wearable data with your input to pinpoint issues like "pain spikes at 2:00 a.m." and offers solutions such as relaxation techniques, timing adjustments, and environmental changes to help you achieve 7–9 hours of rest. For stress, it tracks heart rate variability and breathing patterns, suggesting quick interventions like guided breathing exercises, short walks, or reframing techniques when stress levels rise. For mobility, the app analyzes step counts, sit-stand frequency, and gait smoothness to create activity goals that align with your surgeon's limits. These might include "Stand up once every hour" or "Reach 3,000 steps by the end of week two", with adjustments based on your pain, fatigue, and progress.
Healify also provides smart alerts when sustained changes in your data suggest potential complications. For instance, if your resting heart rate rises, daily step count drops over several days, oxygen levels decrease, or nighttime temperature steadily increases, the app might notify you: "Your heart rate and skin temperature have been elevated for 24 hours, and your activity is down. This could indicate a problem. Contact your surgeon's office or visit urgent care if your symptoms worsen." These alerts are designed to catch issues early without overwhelming you with unnecessary notifications, ensuring peace of mind as you recover at home.
Challenges of AI-Powered Monitoring Systems
Technical and Clinical Limitations
AI-driven wearables often face hurdles in accuracy due to motion artifacts and poor sensor contact, which can lead to false alarms. Issues like limited battery life and unreliable connectivity can further disrupt the timely transmission of critical data.
On the clinical side, validation remains a challenge. For instance, a systematic review of wearables used after abdominal surgery revealed significant variations in devices, metrics, and study methods. The review concluded there is "insufficient high‑quality evidence to support routine clinical use" [9]. Many algorithms are trained on small, single-center datasets, which can limit their effectiveness in broader, more diverse settings. This often forces clinicians to double-check wearable data with bedside measurements or even disregard alerts when confidence in the system wanes.
False positives can overwhelm nursing staff with unnecessary alerts, while false negatives might miss critical signs of complications like sepsis, bleeding, or respiratory failure. To address these issues, hospitals can adjust alert thresholds and implement tiered notifications to reduce alarm fatigue. However, these solutions require continuous fine-tuning and staff training to be effective.
Privacy and Data Security Issues
Beyond technical challenges, protecting patient data adds another layer of complexity.
Continuous monitoring generates a steady stream of sensitive information - such as vital signs, sleep patterns, mobility, and even location - that offers detailed insights into a patient’s health. As this data moves between hospital systems, cloud platforms, consumer wearables, and mobile apps, it passes through multiple hands, including device manufacturers, cloud providers, analytics companies, and app developers. This increases the risk of unauthorized access or misuse.
In the United States, HIPAA requires healthcare organizations and their partners to safeguard protected health information by encrypting data, enforcing strict access controls, and maintaining detailed access logs. However, weak security measures - like poor authentication protocols or unclear data-sharing practices - can lead to compliance issues and put patient privacy at risk. To mitigate these risks, hospitals must establish strong vendor agreements, conduct regular security audits, and maintain clear incident-response plans.
Access and Affordability Barriers
Economic and infrastructure challenges also limit the widespread use of AI-powered monitoring systems.
The upfront cost of hardware, such as patches, smartwatches, and sensors, can range from tens to hundreds of dollars per patient, depending on whether the devices are disposable or reusable. Recurring expenses for software licenses, cloud hosting, EHR integration, technical support, staff training, and workflow adjustments add to the financial strain. Without clear reimbursement policies from Medicare, Medicaid, or private insurers, hospitals may hesitate to invest in these technologies, leaving patients to shoulder potential out-of-pocket expenses.
Reliable infrastructure is another critical factor. Real-time data uploads require consistent broadband or cellular coverage, yet rural areas and some urban, low-income neighborhoods often lack reliable connectivity. Patients also need compatible smartphones - like an iPhone for syncing with certain wearables such as Healify - which creates an additional barrier for those without the necessary devices. Older adults, individuals with cognitive impairments, or those with limited digital literacy may struggle with tasks like charging devices, wearing them correctly, or troubleshooting connectivity issues. These challenges can lead to poor data quality or early abandonment of the technology. Language barriers and poorly designed interfaces that don’t align with diverse user needs further reduce engagement among minority populations, deepening the digital divide. As a result, patients with better resources gain access to advanced monitoring, while others are left with traditional, less frequent follow-ups.
Addressing these obstacles is crucial to unlocking the full potential of AI in improving post-surgical care and recovery outcomes.
What's Next for AI in Post-Surgery Monitoring
Moving from Monitoring to Prediction
AI is steadily evolving from a tool for reactive monitoring to one that can proactively predict complications before they become severe. This shift could redefine how post-surgery care is managed.
Future AI-driven wearables are expected to predict complications hours before they show obvious clinical signs. These systems will adapt to each patient by learning their unique baseline metrics and considering factors like the type of surgery, medications, and existing health conditions [6].
Studies suggest that AI systems can detect complications earlier than traditional monitoring methods, which could lead to fewer ICU transfers, shorter hospital stays, and reduced readmissions [2]. In the U.S., these tools are likely to integrate seamlessly with early warning systems and electronic health records (EHRs), enabling care teams to act based on risk forecasts rather than waiting for emergencies to arise.
Some of the primary areas where AI could make a difference include identifying infections and sepsis by analyzing subtle changes in temperature, heart rate, and variability. It could also predict cardiorespiratory issues such as arrhythmias and hypoxia, thromboembolic events linked to immobility, and even pain flares that could slow recovery [6]. AI platforms are already being used to identify patients at high risk for acute kidney injury, guiding targeted interventions [5]. These advancements could help tailor discharge plans, follow-up schedules, and home care support to each patient’s specific needs.
New Technologies on the Horizon
The next wave of innovation is set to go beyond the familiar smartwatches and chest patches, bringing monitoring closer to the surgical site itself. For instance, smart wound dressings equipped with sensors will monitor local factors like temperature, pH levels, moisture, and biochemical markers. These dressings could even release medication automatically if they detect an infection or other complications [3].
Implantable sensors are another exciting development. Orthopedic and cardiac devices embedded with strain, pressure, or motion sensors could keep tabs on implant stability, detect early signs of failure, and track rehabilitation progress. These sensors would allow AI systems to differentiate between normal recovery and potential problems [5]. Additionally, advanced multi-sensor patches and smart textiles are being developed to continuously measure vital signs, feeding real-time data into recovery and risk assessments [6].
These technologies will likely integrate with consumer devices like the Apple Watch and Fitbit. AI platforms will act as the central hub, synthesizing data from clinical-grade patches, smart dressings, and consumer wearables into streamlined dashboards for healthcare providers. On the patient side, apps like Healify are already combining wearable, biometric, and lifestyle data to offer 24/7 personalized recovery guidance. These apps can provide actionable advice - such as setting daily walking goals, sending wound-care reminders, or suggesting breathing exercises - and issue alerts when concerning trends appear [4]. Such tools are paving the way for broader adoption in clinical practice.
Research and Implementation Needs
For these advancements to become a routine part of postoperative care, rigorous research and thoughtful implementation strategies are essential. Large-scale, multicenter trials across diverse U.S. hospitals will be needed to confirm that AI-enhanced devices actually reduce complications, hospital stays, ICU transfers, and mortality rates [10]. Predictive models must also undergo external validation, including subgroup analyses that account for factors like age, race, ethnicity, socioeconomic status, and preexisting conditions to minimize bias [4].
Cost-effectiveness will also play a critical role. Studies must weigh the expenses of devices, data infrastructure, and staffing against the potential savings from fewer complications and reduced hospital utilization [2]. Additionally, human factors like patient adherence, device comfort, alarm fatigue, and clinician workload must be addressed to ensure these technologies are practical and effective.
Hospitals will need clear protocols to determine which patients should use these devices and for how long - such as 7 to 30 days post-discharge. Thresholds for triggering interventions, whether through nursing calls, telehealth appointments, or in-person evaluations, should be well-defined. Establishing dedicated remote monitoring teams, such as telemetry nurses or advanced practice providers, will be crucial for managing AI alerts and coordinating follow-up care. By integrating these predictive systems into existing EHR workflows and focusing on proactive monitoring rather than adding more alarms, healthcare systems can significantly improve patient recovery and streamline postoperative care. This shift toward predictive, data-driven care has the potential to transform the way hospitals approach recovery and risk management.
Is This the Future of Patient Care? Remote Patient Monitoring, Wearables & AI
Conclusion: Better Recovery Through AI Wearables
AI-powered wearables are revolutionizing post-surgery care by offering continuous, real-time monitoring that catches complications early and tailors recovery plans to each patient. These devices track vital metrics like heart rate, oxygen levels, temperature, mobility, sleep, and pain, ensuring a personalized approach to recovery. Studies have shown that this level of early detection leads to better outcomes for patients.
By analyzing a patient’s baseline data, AI can fine-tune recovery goals - adjusting activity levels, rest periods, and alert thresholds based on factors like age, type of surgery, and overall health. This means patients receive specific, actionable recommendations that help them rebuild strength and confidence during their recovery journey.
For patients recovering at home in the U.S., Healify makes this cutting-edge technology accessible and easy to use. It connects seamlessly with Apple-compatible wearables, analyzing vital signs, activity patterns, sleep quality, and stress levels. The app then translates this data into simple daily tasks, such as "Take 3,000 steps today in smaller intervals" or "Your sleep has been under 6 hours for three nights - here’s how to improve it." Healify’s 24/7 AI health coach, Anna, provides clear recovery guidance, flags potential issues, and prompts users to reach out to their care team when necessary. By combining precise data tracking with actionable insights, Healify demonstrates how technology is transforming post-surgery care into a safer, more personalized experience.
FAQs
How can AI wearables help detect post-surgery complications earlier?
AI-powered wearables bring a new level of convenience and precision to health monitoring by tracking vital signs, stress levels, and other important health metrics in real time. They don’t just collect data - they analyze it to spot subtle changes, like an irregular heartbeat or a spike in stress hormones, long before symptoms become apparent.
This ability to catch early warning signs means quicker intervention, potentially stopping small issues from turning into major health concerns. These devices do more than just inform - they enable patients and healthcare providers to make timely, well-informed decisions that can significantly impact recovery.
What kind of data do AI-powered wearables collect to tailor recovery plans?
AI-powered wearables collect a wide range of health data to design recovery plans tailored to individual needs. They track activity levels, sleep quality, stress markers, hydration levels, and biometric details like heart rate and cortisol levels.
With this data, these devices provide real-time insights and practical feedback, helping users improve recovery and enhance their overall well-being.
What challenges come with using AI-powered wearables for post-surgery monitoring?
Implementing AI-powered wearables in post-surgery care comes with its own set of hurdles. Data privacy tops the list, as handling sensitive health information requires airtight security measures. On top of that, integrating these devices into current healthcare systems can be a tricky and time-intensive process.
Another critical factor is ensuring the accuracy and reliability of the AI algorithms. False alarms or overlooked issues could compromise patient safety and trust. Speaking of trust, patient acceptance of these technologies is essential for their widespread adoption. Lastly, effectively managing the flood of real-time data these devices generate - without overwhelming healthcare teams or patients - is a challenge that cannot be ignored.
Related Blog Posts
Endlich die Kontrolle über Ihre Gesundheit übernehmen

Endlich die Kontrolle über Ihre Gesundheit übernehmen

Endlich die Kontrolle über Ihre Gesundheit übernehmen





