Improve your health
Improve your health
Improve your health
7. Januar 2026
Wearable Data in Telehealth Consultations


Wearable devices are reshaping telehealth by providing continuous, real-time health data. Unlike traditional telehealth that relies on self-reported information, wearables like smartwatches, glucose monitors, and ECG patches offer objective insights into heart rhythms, blood oxygen levels, glucose trends, and more. This data improves chronic disease management, early intervention, and patient outcomes while streamlining provider workflows.
Key points:
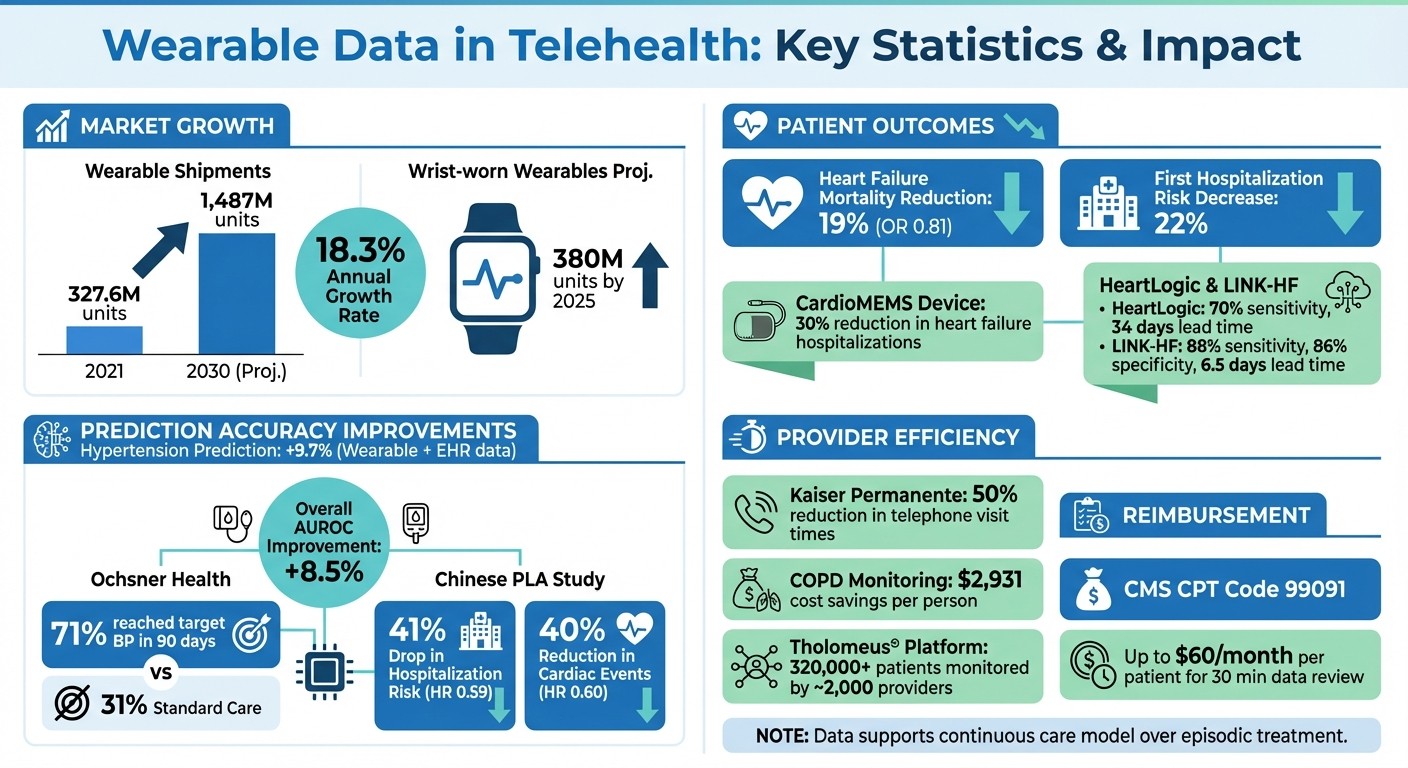
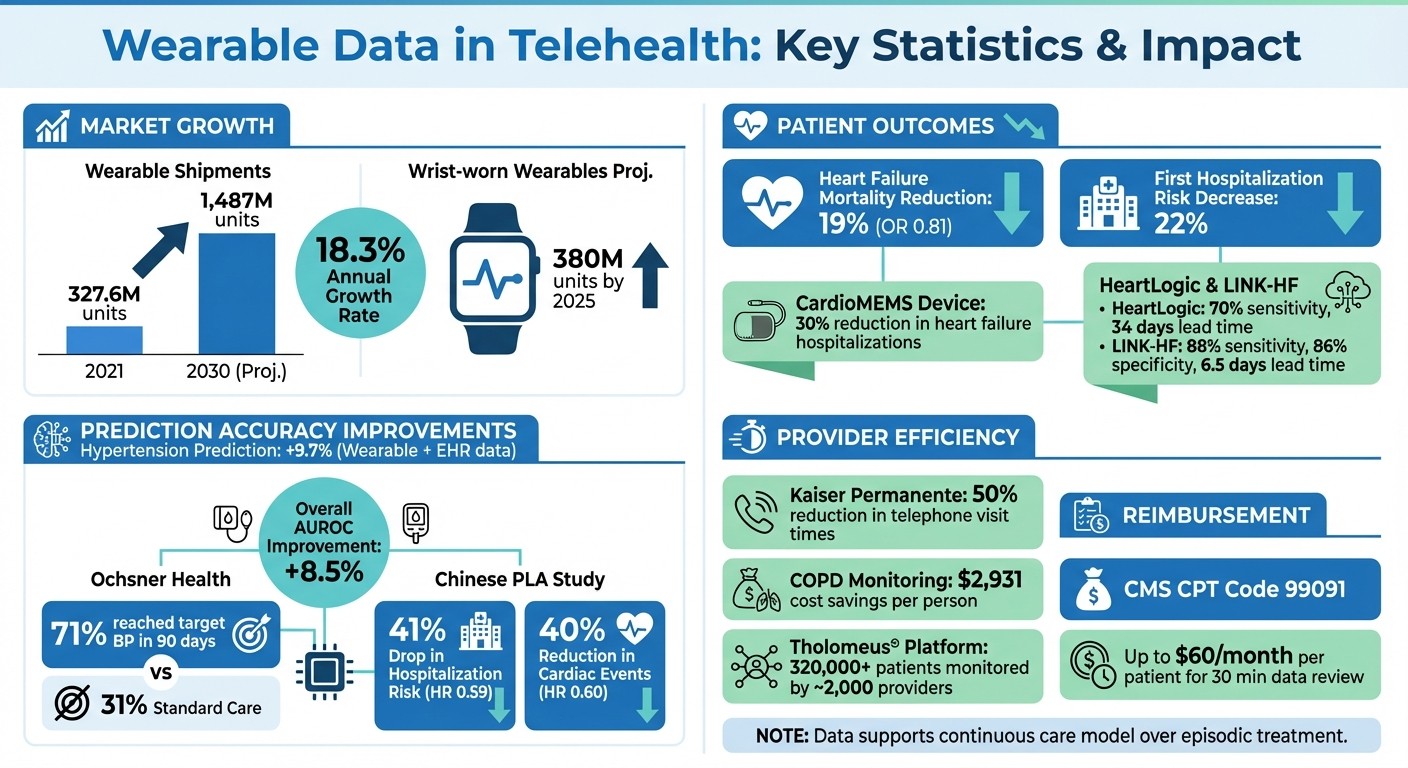
Market Growth: Wearable shipments are projected to grow from 327.6 million units in 2021 to 1.487 billion by 2030.
Improved Predictions: Combining wearable data with EHRs enhances prediction accuracy for conditions like hypertension (+9.7%) and diabetes (+12.6%).
Chronic Disease Impact: Devices like CardioMEMS reduce heart failure hospitalizations by 30%, and CGMs optimize diabetes care.
Provider Efficiency: Automated data collection reduces manual work, while AI tools detect health changes from patients' unique baselines.
Privacy Challenges: Regulatory gaps and cybersecurity risks need addressing to protect wearable data.
Wearables are enabling proactive healthcare, empowering patients and improving provider efficiency, but ensuring data privacy and integration with existing systems remains critical.
Wearable Technology Impact on Telehealth: Key Statistics and Outcomes
What Is Telehealth Integration For Wearable Health Tech Devices? - Talking Tech Trends
Impact on Patient Outcomes
Remote monitoring through wearable devices has shown impressive results, including a 19% reduction in heart failure mortality (odds ratio 0.81) and a 22% decrease in the risk of first hospitalization [5].
Better Management of Chronic Diseases
For patients with chronic conditions, continuous monitoring offers substantial benefits. Take heart failure, for instance. The CardioMEMS device, which tracks pulmonary artery pressure daily, has been proven to lower heart failure-related hospitalizations by 30% in patients with moderately severe symptoms [7]. Another example is the HeartLogic algorithm, which can detect signs of heart failure decompensation with 70% sensitivity and provides a median lead time of 34 days before clinical events occur [7].
In diabetes care, continuous glucose monitors (CGMs) combined with AI-driven tools are transforming how patients manage their condition. For example, DreaMed Diabetes developed a system that analyzes data from CGMs and insulin pumps to deliver personalized insulin titration recommendations for young people with type 1 diabetes [6]. Similarly, the Ochsner Health System implemented a remote patient monitoring (RPM) program for hypertension between 2016 and 2017. By combining digital tools with clinical staff oversight, they achieved better blood pressure control outcomes [6].
The integration of technology with education is a game-changer. RPM programs that incorporate self-management training and educational modules significantly reduce heart failure-related hospitalizations compared to monitoring alone. Adding video communication tools further decreases both disease-specific and overall hospitalizations [5]. These advancements enable healthcare providers to intervene earlier and more effectively.
Preventive Care and Early Intervention
Wearable devices are revolutionizing healthcare by shifting the focus from reactive treatments to proactive care. Continuous monitoring allows for the early detection of warning signs. For instance, the LINK-HF trial, published in May 2021, demonstrated the power of this approach. Using a multisensor patch, researchers monitored 100 heart failure patients and employed a machine learning algorithm that predicted impending decompensation with 88% sensitivity and 86% specificity, offering a median lead time of 6.5 days before clinical events occurred [7].
"RPM technologies have the potential to enable and accelerate a transition from episodic to continuous care." – Devin M. Mann, MD, MS, NYU Grossman School of Medicine [6]
This continuous care model is particularly effective in catching arrhythmias and hypoglycemic episodes before they become critical [8][4]. AI-powered tools can even identify left ventricular systolic dysfunction from ECG data with 74% sensitivity and 87% specificity, allowing for timely interventions in cardiac care [7]. Platforms like Healify (https://healify.ai) utilize wearable data to provide real-time health alerts and personalized recommendations, empowering users to address potential health issues before they escalate.
Improving Provider Efficiency
Wearable technology isn't just improving patient outcomes - it’s also streamlining the way healthcare providers work, especially during telehealth consultations. By automating the collection and analysis of health data, wearables eliminate the need for clinicians to spend time on manual documentation. Instead of relying on patients to remember and report their health metrics, wearables send this information directly to web portals or mobile apps. This gives providers easy access to real-time data, making their workflows more efficient and freeing up time to focus on patient care.
AI-Driven Insights for Providers
Beyond simplifying data collection, wearable devices are now leveraging advanced analytics to support clinical decision-making. AI algorithms analyze continuous streams of data from wearables to spot changes in a patient’s health that might otherwise go unnoticed. Unlike rigid thresholds that can trigger unnecessary alarms, these algorithms detect meaningful shifts from a patient’s unique baseline - such as irregular heart rhythms or worrisome blood pressure trends. This allows providers to identify high-risk patients quickly and deliver timely care during telehealth visits.
Integrating wearable data with electronic health records (EHRs) takes this a step further. By combining continuous lifestyle data with traditional medical records, providers gain a more comprehensive view of a patient’s health between appointments. This enhanced perspective improves risk stratification and triage, helping clinicians make better-informed decisions.
"The fewer places that clinicians have to look for information the more likely it is to be transmitted meaningfully to impact patient care" [9].
Better Care Coordination
Wearable data also fosters better teamwork among healthcare providers. Real-time, shared data enables primary care physicians and specialists to collaborate more effectively, streamlining treatment plans and avoiding redundant tests or delays. Telehealth consultations further enhance this collaboration by connecting on-site providers with off-site specialists, ensuring that medical expertise can be utilized efficiently across different locations [10].
The financial impact is noteworthy too. Remote patient monitoring for conditions like COPD has shown cost savings of $2,931 per person [2]. To fully realize these benefits, health systems need to adopt interoperable standards for seamless data sharing. Employing digital navigators - specialized staff who assist patients with setting up and troubleshooting devices - can also help reduce the technical burden on clinical teams [9]. Platforms like Healify (https://healify.ai) are making strides in this area by integrating wearable data with AI-driven insights, providing both patients and providers with actionable health information in one centralized hub.
These advancements are setting the stage for wearable technology to become an even more integral part of telehealth, enhancing both patient care and provider efficiency.
Technology Advances in Wearable Integration
New Technologies in Wearables
The rapid growth in wearable technology is reshaping both the market and telehealth applications. In fact, the wearable sensor market is projected to jump from 327.6 million units in 2021 to 1,487 million by 2030, with an impressive annual growth rate of 18.3% [11]. What's driving this? New advancements are making wearables more precise, user-friendly, and clinically impactful.
Materials like graphene, MXenes, and black phosphorus are leading the charge for the next generation of skin-integrated sensors. These ultra-thin, flexible materials are highly sensitive, enabling devices to pick up subtle physiological signals such as vocal cord vibrations or arterial pulses. On top of that, hybrid multimodal sensors are now capable of capturing both physical data - like heart rate and gait - and biochemical markers, including glucose and lactate levels in sweat. This dual capability provides a more comprehensive picture of real-time health.
Another game-changer is multi-sensor fusion. Modern wearables combine data from multiple sources, like accelerometers, gyroscopes, optical sensors, and barometric pressure sensors, to create a detailed snapshot of a patient’s activity and physiology. Thanks to standardized protocols like Fast Healthcare Interoperability Resources (FHIR) and Blue Button APIs, platforms such as Apple HealthKit can now integrate wearable data directly into electronic health records. This seamless connection ensures secure and efficient sharing of information, paving the way for real-world applications that are already revolutionizing telehealth.
Real-World Examples of Wearable Integration
The impact of these advancements is already evident in real-world studies. Take the Apple Heart & Movement Study, for example. Launched in November 2019 by Brigham and Women's Hospital and the American Heart Association, this study uses the Apple Watch to gather extensive physiological data. By November 2021, data from 82,809 participants had been analyzed, including over 1.1 million ECGs shared via the FHIR-compliant HealthKit framework [12].
Another compelling example comes from a randomized controlled trial conducted at the Chinese PLA General Hospital between January 2020 and June 2021. This study involved 1,248 elderly patients with chronic coronary heart disease. Participants were equipped with wearables like blood pressure monitors, glucose meters, and 24-hour ambulatory ECG devices. The results were striking: those managed with wearable telemedical monitoring saw a 41% drop in hospitalization risk (HR 0.59) and a 40% reduction in major adverse cardiac events (HR 0.60) compared to traditional care [14].
The TEL-HEMATO Study, conducted at the Institut Català d'Oncologia in Barcelona from November 2022 to July 2023, offers another glimpse into the potential of wearables. Eleven patients undergoing CAR T-cell therapy and hematopoietic cell transplantation were monitored using a Withings ScanWatch and a digital thermometer. Their daily vital signs were integrated into a web-based dashboard for hematologists. While adherence to automated heart rate and SpO2 monitoring was high - 89% and 100% respectively - manual temperature recording fell to 44% by the third month, highlighting the clear benefits of automated data collection [13].
Wearable integration is also boosting telehealth platforms. One example is Healify (https://healify.ai), an AI-driven health coaching app for iPhone users. By incorporating real-time wearable data, Healify delivers personalized health guidance, making virtual consultations more effective and improving outcomes for both patients and providers. These examples underline how wearables are not just gadgets - they’re reshaping healthcare delivery.
Challenges and Future Directions
Addressing Data Privacy and Security Concerns
One of the biggest challenges in using wearable data for telehealth lies in navigating regulatory and security gaps. While HIPAA provides guidelines for healthcare providers and insurance plans, it doesn’t cover many consumer wearable manufacturers. This leaves a fragmented system where state laws and the Federal Trade Commission (FTC) step in to regulate data privacy instead of relying on uniform medical privacy standards [16][17]. For instance, states like Washington and California have taken steps to address this issue. Washington’s My Health My Data Act and California’s CPRA broaden the definition of "consumer health data", including any information that could infer physical or mental health conditions [19]. These laws even prohibit practices like geofencing near mental health clinics to prevent tracking behaviors linked to treatment-seeking [19].
On top of privacy concerns, cybersecurity risks are a major issue. Wearable devices are vulnerable to threats like ransomware, DDoS attacks, and man-in-the-middle exploits during data transmission. To address this, the FDA requires digital health technologies to be rigorously verified and validated before they are used clinically [18]. Additionally, practices like data minimization - where only essential information is collected and retained - can help lower both regulatory and security risks [19]. New state laws that allow individuals to take legal action for health data privacy violations further underscore the importance of clear, user-friendly privacy policies and robust opt-in systems [19]. Tackling these challenges is critical as wearable data becomes increasingly integrated with electronic health records (EHRs), opening doors to better predictive analytics and more efficient care.
Future Trends in Wearable Data and Telehealth
Looking ahead, the future of wearable data in telehealth is all about deeper integration and expanded capabilities for healthcare providers. A key development is the merging of wearable technology with EHRs. By combining continuous data from wearables with EHR information, healthcare providers can get a more complete picture of a patient’s health. This approach has already shown promise in improving predictions for chronic conditions like diabetes and hypertension. In fact, integrating wearable features with EHR data has been shown to boost outcome prediction accuracy by 8.5% AUROC [3].
Real-world examples highlight the potential of this integration. At Ochsner Health System, a digital hypertension program that used connected blood pressure monitors synced with EHRs helped 71% of participants reach their target blood pressure within 90 days. For comparison, only 31% of patients achieved similar results with standard care [15]. Kaiser Permanente also reported success with its digital glucose monitoring program, which reduced telephone visit times by 50%, effectively doubling the capacity of clinicians to manage patient loads [15].
However, the success of these technologies depends on more than just cutting-edge devices - it also requires strong human support systems. Many healthcare organizations are setting up tech bars to help patients with device setup and app downloads, easing the burden on clinicians [15]. Personalized coaching and support teams are also playing a role in combating "wearable fatigue", where patients stop using devices after just a few months [15].
On the financial side, evolving reimbursement models are making it easier for providers to embrace wearable data. For example, CMS CPT code 99091 allows providers to bill up to $60 per month per patient for spending 30 minutes reviewing wearable data [15]. Platforms like Healify (https://healify.ai) are stepping in to support these models by using AI-driven analytics to turn raw wearable data into actionable insights, offering 24/7 personalized health coaching for patients and valuable data for providers.
Conclusion
Wearable technology is transforming telehealth by enabling continuous care, improving patient outcomes, and boosting efficiency for healthcare providers. For individuals managing chronic conditions like diabetes or heart disease, these devices offer real-time feedback, empowering better self-care and facilitating earlier interventions. On the provider side, AI-driven insights help prioritize high-risk cases and minimize time spent on manual data analysis, allowing clinicians to focus on diagnosis and treatment.
The integration of wearables also strengthens predictive analytics. A notable example is the Tholomeus® platform, which has successfully monitored over 320,000 patients with the involvement of approximately 2,000 healthcare professionals. This illustrates the scalability and impact of wearable technology in healthcare [20]. As Dr. Sneha S. Jain from Stanford Health Care notes:
The bond between technology and clinical medicine is only getting stronger. Medicine must evolve to meet patients where they are [21].
Yet, realizing the full potential of wearables in telehealth requires tackling significant challenges. Data privacy and security are pressing concerns, and the lack of transparency in AI algorithms can erode clinician trust. Building trust will depend on creating AI systems that are both transparent and explainable [1].
Future research must address these issues by focusing on improving AI transparency, diversifying datasets, and ensuring seamless integration of wearable data. For instance, only 7% of studies combining AI and wearables for diabetes management have reported racial and ethnic demographics - an essential gap that must be closed [1]. Platforms like Healify (https://healify.ai) are working to bridge this divide by turning raw wearable data into actionable insights through AI-powered coaching, making complex health information more accessible for everyday users.
As wearable technology advances, it holds the potential to revolutionize telehealth by providing clinically validated, equitable care. With wrist-worn wearable shipments projected to hit 380 million units by 2025 [21], the infrastructure is growing rapidly. Continued investment in research and development will ensure these devices deliver trustworthy and meaningful outcomes for all patients.
FAQs
How do wearable devices improve telehealth consultations?
Wearable devices are transforming telehealth by delivering real-time health data, like heart rate, blood pressure, oxygen levels, physical activity, and sleep patterns. This steady flow of information gives healthcare providers a clearer, more detailed picture of your health without needing frequent in-person visits or additional monitoring tools.
By using data from wearables, providers can spot potential health issues earlier, fine-tune treatments, and ensure better medication compliance. This approach helps manage chronic conditions more effectively, reduces hospital visits, and boosts patient satisfaction. For individuals at higher risk, remote monitoring adds an extra layer of safety while cutting down on unnecessary trips to the doctor.
On top of that, automated data collection from wearables frees up clinicians' time, allowing them to focus more on patient care instead of tedious manual data entry. As regulations for AI-powered devices continue to evolve, wearable technology is making telehealth more efficient and tailored to individual needs, offering a practical and modern alternative to traditional healthcare appointments.
What are the privacy risks of using wearable devices in telehealth?
Privacy concerns surrounding wearable devices stem from the fact that current health privacy laws, such as HIPAA, were created with traditional healthcare systems in mind. These laws don’t fully account for the health data generated by fitness trackers, smartwatches, and health apps. As a result, this data can sometimes end up in the hands of third parties, like advertisers, without proper oversight or user awareness.
In response, federal and state regulations are gradually evolving to close these gaps and offer stronger protections for consumer health data. Despite these efforts, many users remain wary. Unclear consent processes, inconsistent security practices, and the risk of breaches or misuse contribute to this skepticism. Research also reveals that the lack of transparency in how wearable companies manage data can undermine trust - not just for users but also for healthcare providers.
Platforms like Healify aim to address these concerns by prioritizing user privacy. They employ robust encryption, ensure consent workflows are straightforward, and adhere to new regulations, all to keep your data secure and responsibly managed.
How can wearable devices help manage chronic conditions more effectively?
Wearable devices offer a steady stream of health data, including heart rate, activity levels, sleep patterns, blood oxygen levels, and, for some users, even glucose or blood pressure readings. This real-time information allows healthcare providers to keep a closer eye on chronic conditions like diabetes, hypertension, and heart disease. The result? Earlier detection of potential issues and more tailored treatment plans.
Studies have shown that incorporating wearables into chronic care management can lead to better health outcomes and increased efficiency. For instance, wearable technology has been linked to fewer hospital readmissions, improved medication adherence, and quicker identification of health concerns. Apps like Healify take things further by transforming wearable data into actionable insights. By analyzing health metrics and offering around-the-clock personalized recommendations, Healify empowers users to manage their conditions more effectively, make smarter lifestyle choices, and reduce the need for frequent in-person doctor visits.
Related Blog Posts
Wearable devices are reshaping telehealth by providing continuous, real-time health data. Unlike traditional telehealth that relies on self-reported information, wearables like smartwatches, glucose monitors, and ECG patches offer objective insights into heart rhythms, blood oxygen levels, glucose trends, and more. This data improves chronic disease management, early intervention, and patient outcomes while streamlining provider workflows.
Key points:
Market Growth: Wearable shipments are projected to grow from 327.6 million units in 2021 to 1.487 billion by 2030.
Improved Predictions: Combining wearable data with EHRs enhances prediction accuracy for conditions like hypertension (+9.7%) and diabetes (+12.6%).
Chronic Disease Impact: Devices like CardioMEMS reduce heart failure hospitalizations by 30%, and CGMs optimize diabetes care.
Provider Efficiency: Automated data collection reduces manual work, while AI tools detect health changes from patients' unique baselines.
Privacy Challenges: Regulatory gaps and cybersecurity risks need addressing to protect wearable data.
Wearables are enabling proactive healthcare, empowering patients and improving provider efficiency, but ensuring data privacy and integration with existing systems remains critical.
Wearable Technology Impact on Telehealth: Key Statistics and Outcomes
What Is Telehealth Integration For Wearable Health Tech Devices? - Talking Tech Trends
Impact on Patient Outcomes
Remote monitoring through wearable devices has shown impressive results, including a 19% reduction in heart failure mortality (odds ratio 0.81) and a 22% decrease in the risk of first hospitalization [5].
Better Management of Chronic Diseases
For patients with chronic conditions, continuous monitoring offers substantial benefits. Take heart failure, for instance. The CardioMEMS device, which tracks pulmonary artery pressure daily, has been proven to lower heart failure-related hospitalizations by 30% in patients with moderately severe symptoms [7]. Another example is the HeartLogic algorithm, which can detect signs of heart failure decompensation with 70% sensitivity and provides a median lead time of 34 days before clinical events occur [7].
In diabetes care, continuous glucose monitors (CGMs) combined with AI-driven tools are transforming how patients manage their condition. For example, DreaMed Diabetes developed a system that analyzes data from CGMs and insulin pumps to deliver personalized insulin titration recommendations for young people with type 1 diabetes [6]. Similarly, the Ochsner Health System implemented a remote patient monitoring (RPM) program for hypertension between 2016 and 2017. By combining digital tools with clinical staff oversight, they achieved better blood pressure control outcomes [6].
The integration of technology with education is a game-changer. RPM programs that incorporate self-management training and educational modules significantly reduce heart failure-related hospitalizations compared to monitoring alone. Adding video communication tools further decreases both disease-specific and overall hospitalizations [5]. These advancements enable healthcare providers to intervene earlier and more effectively.
Preventive Care and Early Intervention
Wearable devices are revolutionizing healthcare by shifting the focus from reactive treatments to proactive care. Continuous monitoring allows for the early detection of warning signs. For instance, the LINK-HF trial, published in May 2021, demonstrated the power of this approach. Using a multisensor patch, researchers monitored 100 heart failure patients and employed a machine learning algorithm that predicted impending decompensation with 88% sensitivity and 86% specificity, offering a median lead time of 6.5 days before clinical events occurred [7].
"RPM technologies have the potential to enable and accelerate a transition from episodic to continuous care." – Devin M. Mann, MD, MS, NYU Grossman School of Medicine [6]
This continuous care model is particularly effective in catching arrhythmias and hypoglycemic episodes before they become critical [8][4]. AI-powered tools can even identify left ventricular systolic dysfunction from ECG data with 74% sensitivity and 87% specificity, allowing for timely interventions in cardiac care [7]. Platforms like Healify (https://healify.ai) utilize wearable data to provide real-time health alerts and personalized recommendations, empowering users to address potential health issues before they escalate.
Improving Provider Efficiency
Wearable technology isn't just improving patient outcomes - it’s also streamlining the way healthcare providers work, especially during telehealth consultations. By automating the collection and analysis of health data, wearables eliminate the need for clinicians to spend time on manual documentation. Instead of relying on patients to remember and report their health metrics, wearables send this information directly to web portals or mobile apps. This gives providers easy access to real-time data, making their workflows more efficient and freeing up time to focus on patient care.
AI-Driven Insights for Providers
Beyond simplifying data collection, wearable devices are now leveraging advanced analytics to support clinical decision-making. AI algorithms analyze continuous streams of data from wearables to spot changes in a patient’s health that might otherwise go unnoticed. Unlike rigid thresholds that can trigger unnecessary alarms, these algorithms detect meaningful shifts from a patient’s unique baseline - such as irregular heart rhythms or worrisome blood pressure trends. This allows providers to identify high-risk patients quickly and deliver timely care during telehealth visits.
Integrating wearable data with electronic health records (EHRs) takes this a step further. By combining continuous lifestyle data with traditional medical records, providers gain a more comprehensive view of a patient’s health between appointments. This enhanced perspective improves risk stratification and triage, helping clinicians make better-informed decisions.
"The fewer places that clinicians have to look for information the more likely it is to be transmitted meaningfully to impact patient care" [9].
Better Care Coordination
Wearable data also fosters better teamwork among healthcare providers. Real-time, shared data enables primary care physicians and specialists to collaborate more effectively, streamlining treatment plans and avoiding redundant tests or delays. Telehealth consultations further enhance this collaboration by connecting on-site providers with off-site specialists, ensuring that medical expertise can be utilized efficiently across different locations [10].
The financial impact is noteworthy too. Remote patient monitoring for conditions like COPD has shown cost savings of $2,931 per person [2]. To fully realize these benefits, health systems need to adopt interoperable standards for seamless data sharing. Employing digital navigators - specialized staff who assist patients with setting up and troubleshooting devices - can also help reduce the technical burden on clinical teams [9]. Platforms like Healify (https://healify.ai) are making strides in this area by integrating wearable data with AI-driven insights, providing both patients and providers with actionable health information in one centralized hub.
These advancements are setting the stage for wearable technology to become an even more integral part of telehealth, enhancing both patient care and provider efficiency.
Technology Advances in Wearable Integration
New Technologies in Wearables
The rapid growth in wearable technology is reshaping both the market and telehealth applications. In fact, the wearable sensor market is projected to jump from 327.6 million units in 2021 to 1,487 million by 2030, with an impressive annual growth rate of 18.3% [11]. What's driving this? New advancements are making wearables more precise, user-friendly, and clinically impactful.
Materials like graphene, MXenes, and black phosphorus are leading the charge for the next generation of skin-integrated sensors. These ultra-thin, flexible materials are highly sensitive, enabling devices to pick up subtle physiological signals such as vocal cord vibrations or arterial pulses. On top of that, hybrid multimodal sensors are now capable of capturing both physical data - like heart rate and gait - and biochemical markers, including glucose and lactate levels in sweat. This dual capability provides a more comprehensive picture of real-time health.
Another game-changer is multi-sensor fusion. Modern wearables combine data from multiple sources, like accelerometers, gyroscopes, optical sensors, and barometric pressure sensors, to create a detailed snapshot of a patient’s activity and physiology. Thanks to standardized protocols like Fast Healthcare Interoperability Resources (FHIR) and Blue Button APIs, platforms such as Apple HealthKit can now integrate wearable data directly into electronic health records. This seamless connection ensures secure and efficient sharing of information, paving the way for real-world applications that are already revolutionizing telehealth.
Real-World Examples of Wearable Integration
The impact of these advancements is already evident in real-world studies. Take the Apple Heart & Movement Study, for example. Launched in November 2019 by Brigham and Women's Hospital and the American Heart Association, this study uses the Apple Watch to gather extensive physiological data. By November 2021, data from 82,809 participants had been analyzed, including over 1.1 million ECGs shared via the FHIR-compliant HealthKit framework [12].
Another compelling example comes from a randomized controlled trial conducted at the Chinese PLA General Hospital between January 2020 and June 2021. This study involved 1,248 elderly patients with chronic coronary heart disease. Participants were equipped with wearables like blood pressure monitors, glucose meters, and 24-hour ambulatory ECG devices. The results were striking: those managed with wearable telemedical monitoring saw a 41% drop in hospitalization risk (HR 0.59) and a 40% reduction in major adverse cardiac events (HR 0.60) compared to traditional care [14].
The TEL-HEMATO Study, conducted at the Institut Català d'Oncologia in Barcelona from November 2022 to July 2023, offers another glimpse into the potential of wearables. Eleven patients undergoing CAR T-cell therapy and hematopoietic cell transplantation were monitored using a Withings ScanWatch and a digital thermometer. Their daily vital signs were integrated into a web-based dashboard for hematologists. While adherence to automated heart rate and SpO2 monitoring was high - 89% and 100% respectively - manual temperature recording fell to 44% by the third month, highlighting the clear benefits of automated data collection [13].
Wearable integration is also boosting telehealth platforms. One example is Healify (https://healify.ai), an AI-driven health coaching app for iPhone users. By incorporating real-time wearable data, Healify delivers personalized health guidance, making virtual consultations more effective and improving outcomes for both patients and providers. These examples underline how wearables are not just gadgets - they’re reshaping healthcare delivery.
Challenges and Future Directions
Addressing Data Privacy and Security Concerns
One of the biggest challenges in using wearable data for telehealth lies in navigating regulatory and security gaps. While HIPAA provides guidelines for healthcare providers and insurance plans, it doesn’t cover many consumer wearable manufacturers. This leaves a fragmented system where state laws and the Federal Trade Commission (FTC) step in to regulate data privacy instead of relying on uniform medical privacy standards [16][17]. For instance, states like Washington and California have taken steps to address this issue. Washington’s My Health My Data Act and California’s CPRA broaden the definition of "consumer health data", including any information that could infer physical or mental health conditions [19]. These laws even prohibit practices like geofencing near mental health clinics to prevent tracking behaviors linked to treatment-seeking [19].
On top of privacy concerns, cybersecurity risks are a major issue. Wearable devices are vulnerable to threats like ransomware, DDoS attacks, and man-in-the-middle exploits during data transmission. To address this, the FDA requires digital health technologies to be rigorously verified and validated before they are used clinically [18]. Additionally, practices like data minimization - where only essential information is collected and retained - can help lower both regulatory and security risks [19]. New state laws that allow individuals to take legal action for health data privacy violations further underscore the importance of clear, user-friendly privacy policies and robust opt-in systems [19]. Tackling these challenges is critical as wearable data becomes increasingly integrated with electronic health records (EHRs), opening doors to better predictive analytics and more efficient care.
Future Trends in Wearable Data and Telehealth
Looking ahead, the future of wearable data in telehealth is all about deeper integration and expanded capabilities for healthcare providers. A key development is the merging of wearable technology with EHRs. By combining continuous data from wearables with EHR information, healthcare providers can get a more complete picture of a patient’s health. This approach has already shown promise in improving predictions for chronic conditions like diabetes and hypertension. In fact, integrating wearable features with EHR data has been shown to boost outcome prediction accuracy by 8.5% AUROC [3].
Real-world examples highlight the potential of this integration. At Ochsner Health System, a digital hypertension program that used connected blood pressure monitors synced with EHRs helped 71% of participants reach their target blood pressure within 90 days. For comparison, only 31% of patients achieved similar results with standard care [15]. Kaiser Permanente also reported success with its digital glucose monitoring program, which reduced telephone visit times by 50%, effectively doubling the capacity of clinicians to manage patient loads [15].
However, the success of these technologies depends on more than just cutting-edge devices - it also requires strong human support systems. Many healthcare organizations are setting up tech bars to help patients with device setup and app downloads, easing the burden on clinicians [15]. Personalized coaching and support teams are also playing a role in combating "wearable fatigue", where patients stop using devices after just a few months [15].
On the financial side, evolving reimbursement models are making it easier for providers to embrace wearable data. For example, CMS CPT code 99091 allows providers to bill up to $60 per month per patient for spending 30 minutes reviewing wearable data [15]. Platforms like Healify (https://healify.ai) are stepping in to support these models by using AI-driven analytics to turn raw wearable data into actionable insights, offering 24/7 personalized health coaching for patients and valuable data for providers.
Conclusion
Wearable technology is transforming telehealth by enabling continuous care, improving patient outcomes, and boosting efficiency for healthcare providers. For individuals managing chronic conditions like diabetes or heart disease, these devices offer real-time feedback, empowering better self-care and facilitating earlier interventions. On the provider side, AI-driven insights help prioritize high-risk cases and minimize time spent on manual data analysis, allowing clinicians to focus on diagnosis and treatment.
The integration of wearables also strengthens predictive analytics. A notable example is the Tholomeus® platform, which has successfully monitored over 320,000 patients with the involvement of approximately 2,000 healthcare professionals. This illustrates the scalability and impact of wearable technology in healthcare [20]. As Dr. Sneha S. Jain from Stanford Health Care notes:
The bond between technology and clinical medicine is only getting stronger. Medicine must evolve to meet patients where they are [21].
Yet, realizing the full potential of wearables in telehealth requires tackling significant challenges. Data privacy and security are pressing concerns, and the lack of transparency in AI algorithms can erode clinician trust. Building trust will depend on creating AI systems that are both transparent and explainable [1].
Future research must address these issues by focusing on improving AI transparency, diversifying datasets, and ensuring seamless integration of wearable data. For instance, only 7% of studies combining AI and wearables for diabetes management have reported racial and ethnic demographics - an essential gap that must be closed [1]. Platforms like Healify (https://healify.ai) are working to bridge this divide by turning raw wearable data into actionable insights through AI-powered coaching, making complex health information more accessible for everyday users.
As wearable technology advances, it holds the potential to revolutionize telehealth by providing clinically validated, equitable care. With wrist-worn wearable shipments projected to hit 380 million units by 2025 [21], the infrastructure is growing rapidly. Continued investment in research and development will ensure these devices deliver trustworthy and meaningful outcomes for all patients.
FAQs
How do wearable devices improve telehealth consultations?
Wearable devices are transforming telehealth by delivering real-time health data, like heart rate, blood pressure, oxygen levels, physical activity, and sleep patterns. This steady flow of information gives healthcare providers a clearer, more detailed picture of your health without needing frequent in-person visits or additional monitoring tools.
By using data from wearables, providers can spot potential health issues earlier, fine-tune treatments, and ensure better medication compliance. This approach helps manage chronic conditions more effectively, reduces hospital visits, and boosts patient satisfaction. For individuals at higher risk, remote monitoring adds an extra layer of safety while cutting down on unnecessary trips to the doctor.
On top of that, automated data collection from wearables frees up clinicians' time, allowing them to focus more on patient care instead of tedious manual data entry. As regulations for AI-powered devices continue to evolve, wearable technology is making telehealth more efficient and tailored to individual needs, offering a practical and modern alternative to traditional healthcare appointments.
What are the privacy risks of using wearable devices in telehealth?
Privacy concerns surrounding wearable devices stem from the fact that current health privacy laws, such as HIPAA, were created with traditional healthcare systems in mind. These laws don’t fully account for the health data generated by fitness trackers, smartwatches, and health apps. As a result, this data can sometimes end up in the hands of third parties, like advertisers, without proper oversight or user awareness.
In response, federal and state regulations are gradually evolving to close these gaps and offer stronger protections for consumer health data. Despite these efforts, many users remain wary. Unclear consent processes, inconsistent security practices, and the risk of breaches or misuse contribute to this skepticism. Research also reveals that the lack of transparency in how wearable companies manage data can undermine trust - not just for users but also for healthcare providers.
Platforms like Healify aim to address these concerns by prioritizing user privacy. They employ robust encryption, ensure consent workflows are straightforward, and adhere to new regulations, all to keep your data secure and responsibly managed.
How can wearable devices help manage chronic conditions more effectively?
Wearable devices offer a steady stream of health data, including heart rate, activity levels, sleep patterns, blood oxygen levels, and, for some users, even glucose or blood pressure readings. This real-time information allows healthcare providers to keep a closer eye on chronic conditions like diabetes, hypertension, and heart disease. The result? Earlier detection of potential issues and more tailored treatment plans.
Studies have shown that incorporating wearables into chronic care management can lead to better health outcomes and increased efficiency. For instance, wearable technology has been linked to fewer hospital readmissions, improved medication adherence, and quicker identification of health concerns. Apps like Healify take things further by transforming wearable data into actionable insights. By analyzing health metrics and offering around-the-clock personalized recommendations, Healify empowers users to manage their conditions more effectively, make smarter lifestyle choices, and reduce the need for frequent in-person doctor visits.
Related Blog Posts
Endlich die Kontrolle über Ihre Gesundheit übernehmen

Endlich die Kontrolle über Ihre Gesundheit übernehmen

Endlich die Kontrolle über Ihre Gesundheit übernehmen





