Improve your health
Improve your health
Improve your health
12 de diciembre de 2025
Consentimiento Dinámico vs. Consentimiento Tradicional: Principales Diferencias


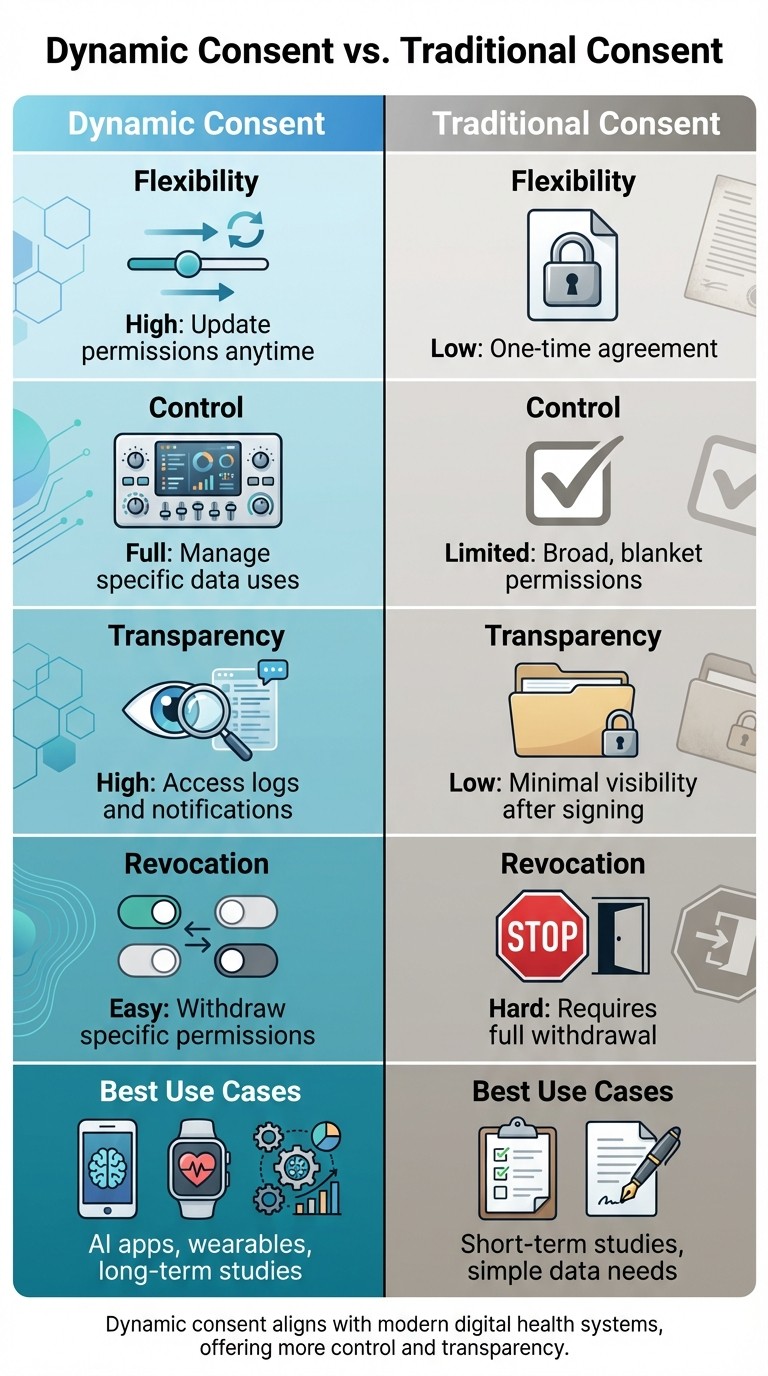
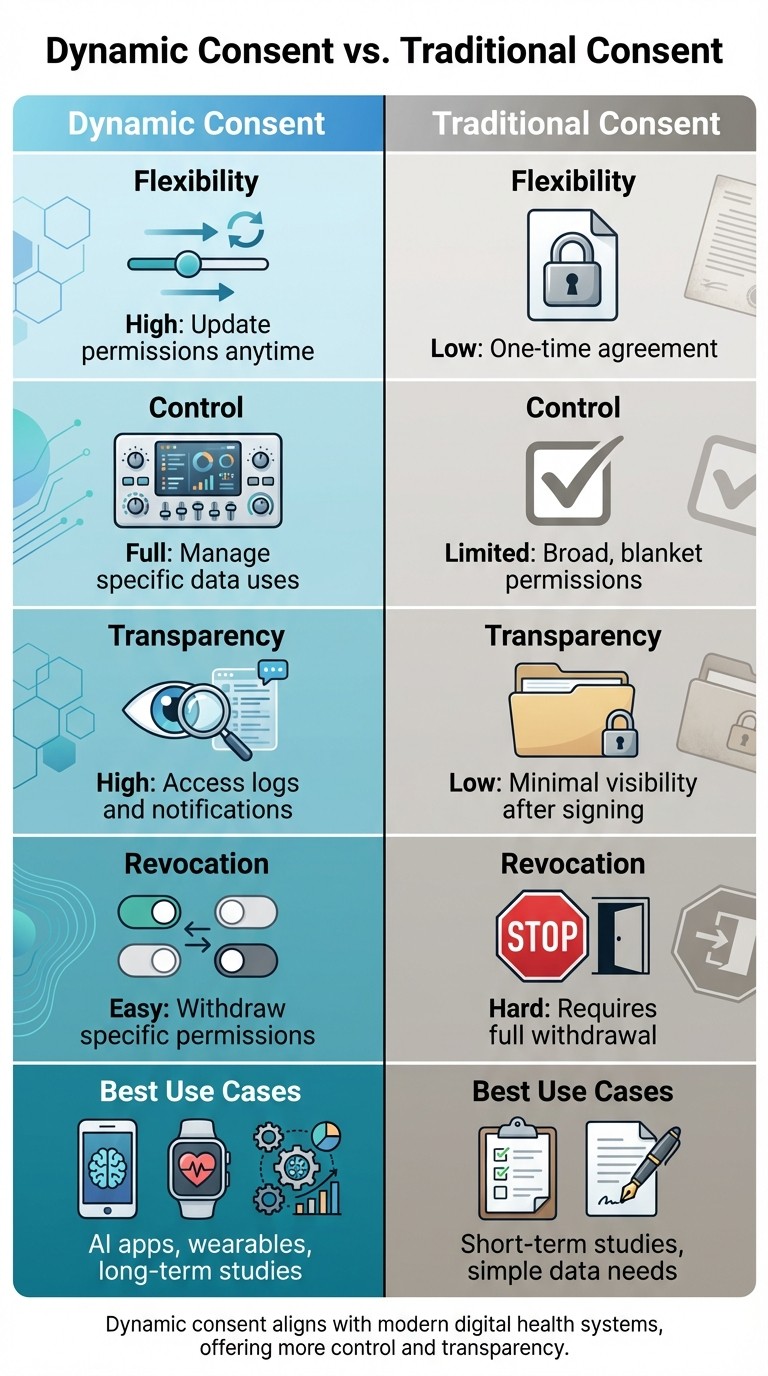
El consentimiento es la forma en que controlas quién usa tus datos de salud y con qué propósito. El consentimiento dinámico te ofrece un control continuo a través de herramientas digitales, mientras que el consentimiento tradicional es un acuerdo único con flexibilidad limitada. Aquí tienes un resumen rápido:
Consentimiento Dinámico: Te permite actualizar permisos en cualquier momento a través de una plataforma segura. Puedes gestionar usos específicos de datos, retirar selectivamente los permisos y hacer un seguimiento de quién accede a tus datos.
Consentimiento Tradicional: Implica la firma de un formulario amplio y estático. Los cambios requieren la retirada completa, y rara vez ves cómo se utilizan tus datos.
El consentimiento dinámico es ideal para aplicaciones de salud modernas y estudios a largo plazo donde el uso de datos evoluciona, mientras que el consentimiento tradicional funciona para necesidades más simples y a corto plazo.
Comparación Rápida
Característica | Consentimiento Dinámico | Consentimiento Tradicional |
|---|---|---|
Flexibilidad | Alta: Actualiza permisos en cualquier momento | Baja: Acuerdo único |
Control | Completo: Gestiona usos específicos de datos | Limitado: Permisos amplios y generales |
Transparencia | Alta: Acceso a registros y notificaciones | Baja: Visibilidad mínima tras la firma |
Revocación | Fácil: Retira permisos específicos | Difícil: Requiere retirada completa |
Mejores Casos de Uso | Aplicaciones de IA, dispositivos portátiles, estudios a largo plazo | Estudios a corto plazo, necesidades de datos simples |
El consentimiento dinámico se alinea con los sistemas de salud digital actuales, ofreciendo más control y transparencia. El consentimiento tradicional es más simple pero menos adecuado para un uso de datos en evolución.
Consentimiento Dinámico vs Consentimiento Tradicional: Tabla de Comparación de Características
Consentimiento Dinámico
¿Qué es el Consentimiento Tradicional?
El consentimiento tradicional es un acuerdo fijo, único donde las personas otorgan un permiso amplio para el uso de sus datos de salud, a menudo con una sola firma.
Características del Consentimiento Tradicional
En este modelo, los pacientes firman formularios que permiten el acceso a sus biospecímenes y registros de salud para propósitos futuros no especificados. Normalmente, este proceso se basa en métodos en papel o sistemas electrónicos básicos. Sin embargo, carece de la flexibilidad para ajustarse a objetivos de investigación en evolución o nuevos usos para los datos [1].
Fortalezas del Consentimiento Tradicional
La simplicidad del consentimiento tradicional lo hace fácil de implementar y ampliamente accesible. El proceso es directo: los participantes leen un formulario, lo firman, y su participación está confirmada. Esta simplicidad se traduce en menores costos para las organizaciones y asegura accesibilidad para individuos que pueden no usar plataformas digitales. Históricamente, los formularios de consentimiento en papel fueron el método preferido para biobancos y ensayos clínicos antes de que los modelos de consentimiento dinámico estuvieran disponibles [1].
Limitaciones del Consentimiento Tradicional
Una de las mayores desventajas del consentimiento tradicional es su rigidez. Los participantes que se sientan incómodos con ciertos aspectos de un estudio deben retirarse por completo, ya que el modelo no permite ajustes selectivos a los permisos. Una vez dado el consentimiento, no hay forma de actualizar preferencias o revocar permisos específicos sin abandonar el estudio por completo. Este enfoque todo-o-nada puede desalentar la participación continua y puede no respetar completamente la autonomía del participante a medida que la investigación evoluciona.
Además, el consentimiento tradicional no se alinea bien con los sistemas digitales modernos, como aplicaciones de salud impulsadas por IA o dispositivos portátiles que recopilan datos continuamente. Estas tecnologías requieren permisos más detallados y auditorías más robustas para cumplir con regulaciones como HIPAA y GDPR [1]. Esta falta de adaptabilidad ha dado paso a modelos de consentimiento dinámico, que proporcionan opciones más flexibles y continuas para los participantes.
¿Qué es el Consentimiento Dinámico?
El consentimiento dinámico es una forma moderna e interactiva de gestionar cómo se usa tu información de salud. En lugar de firmar un formulario de consentimiento único que cubra todos los posibles usos, este enfoque te ofrece un control continuo. A través de una plataforma digital segura, puedes actualizar tus preferencias en cualquier momento, adaptando los permisos a medida que tu nivel de comodidad o circunstancias evolucionan.
Este sistema prioriza la comunicación en tiempo real entre tú y las organizaciones que usan tus datos. Te permite decidir, en detalle, quién puede acceder a tu información, qué datos pueden usar, y con qué propósitos - todo con la capacidad de ajustar estas configuraciones instantáneamente.
Características Clave del Consentimiento Dinámico
Una de las características destacadas del consentimiento dinámico es su panel de usuario amigable. Este panel muestra tus permisos actuales y te permite optar por o en contra con un solo clic. Cualquier cambio que realices se aplica inmediatamente en todos los sistemas que gestionan tus datos.
El sistema también ofrece un control detallado sobre tus permisos. Por ejemplo, puedes especificar el consentimiento basado en el tipo de datos - ya sea información genómica, datos de dispositivos portátiles, o registros de salud mental. También puedes definir permisos basados en el propósito, como si los datos se usarán para coaching personal, investigación, o fines comerciales, e incluso establecer límites de tiempo para cuánto tiempo se pueden usar tus datos. Para ayudarte a mantenerte informado, la plataforma proporciona notificaciones y recursos educativos sobre nuevos usos de datos.
Tras bambalinas, el sistema mantiene un registro en tiempo real de eventos de acceso a datos y cambios de consentimiento. Estas auditorías aseguran el cumplimiento con regulaciones de privacidad como HIPAA y construyen confianza al documentar cómo se maneja tu información.
Beneficios del Consentimiento Dinámico
El consentimiento dinámico te pone a cargo de tus datos de salud, permitiéndote ajustar permisos sin el enfoque todo-o-nada de los modelos tradicionales. Puedes retirar permisos específicos sin detener todo el intercambio de datos, lo que ayuda a combatir la "fatiga del consentimiento" centralizando todo en un solo lugar.
El formato digital también facilita la comprensión de a qué estás accediendo. Visuales claros y explicaciones sencillas te ayudan a revisar y ajustar configuraciones rápidamente. Para las organizaciones, este enfoque no solo asegura el cumplimiento con las leyes de privacidad, sino que también apoya estudios a largo plazo al mantener a los participantes comprometidos y sintiéndose en control.
Al ofrecer este nivel de flexibilidad y transparencia, el consentimiento dinámico fortalece la confianza y mejora la relación entre los usuarios y las plataformas de salud digital.
Ejemplos de Uso de Consentimiento Dinámico
El consentimiento dinámico ya está causando impacto en la salud digital. Por ejemplo, aplicaciones impulsadas por IA que analizan datos de dispositivos portátiles, biometría, pruebas de sangre y hábitos de vida pueden usar este modelo para darte control completo sobre qué flujos de datos se comparten. Imagina una plataforma como Healify, donde puedes otorgar o revocar acceso a fuentes de datos específicas, como el ritmo cardíaco de tu reloj inteligente, tus patrones de sueño o resultados de laboratorio. También podrías decidir si tus datos desidentificados se usan exclusivamente para coaching personal o si pueden contribuir al desarrollo de algoritmos e investigación.
Este nivel de control garantiza que tus datos se usen de formas que se alinean con tus preferencias, convirtiendo al consentimiento dinámico en un cambio radical en la gestión de salud personalizada.
Diferencias Clave entre el Consentimiento Dinámico y el Tradicional
Tabla de Comparación: Consentimiento Dinámico vs. Consentimiento Tradicional
Cuando comparas el consentimiento dinámico y el tradicional lado a lado, las diferencias son notables. El consentimiento tradicional se basa en un formulario único, a menudo redactado en términos generales, que cubre todos los usos futuros de tus datos y es difícil de modificar. Sin embargo, el consentimiento dinámico ofrece control continuo a través de herramientas digitales, facilitando el ajuste de permisos cuando sea necesario.
Atributo | Consentimiento Dinámico | Consentimiento Tradicional |
|---|---|---|
Flexibilidad | Alta: Actualizaciones en tiempo real con permisos específicos para tipos de datos y plazos | Baja: Formularios estáticos que requieren nueva documentación para cambios |
Control de Participantes | Completo: Paneles digitales te permiten gestionar permisos para usos de datos individuales | Limitado: Permisos amplios y generales con mínima intervención del participante después de firmar |
Comunicación | Interacción continua y bidireccional a través de plataformas seguras con actualizaciones y notificaciones | Conversación única o formulario al inicio |
Revocación | Inmediata y parcial: Retira permisos específicos sin dejar el estudio | Consumo de tiempo y a menudo requiere retirada completa a través de documentación extensa |
Transparencia | Alta: Auditorías detalladas muestran quién accedió a tus datos, cuándo y por qué | Baja: Visibilidad limitada al uso de datos después del primer consentimiento |
Estas diferencias se vuelven más claras al explorarlas a través de escenarios del mundo real.
Comprendiendo las Diferencias con Ejemplos
Toma como ejemplo la investigación de salud a largo plazo. Con el consentimiento dinámico, los participantes pueden ajustar sus permisos con el tiempo. Por ejemplo, alguien podría permitir el uso de sus registros de salud para un estudio específico hoy pero decidir restringir el acceso a ciertos tipos de datos en el futuro. En cambio, el consentimiento tradicional bloquea a los participantes en un acuerdo "todo-o-nada", ofreciendo ninguna flexibilidad para refinar sus elecciones más tarde.
El control del participante es otra diferencia clave. Las plataformas de consentimiento dinámico empoderan a los usuarios para tomar decisiones precisas, como aprobar el uso de datos biométricos pero declinar el uso de información genética. Estas plataformas también proporcionan registros de acceso para que los participantes puedan ver exactamente cómo se utilizan sus datos. Por otro lado, los formularios de consentimiento tradicional a menudo utilizan un lenguaje vago, dejando a los participantes con poca información o control una vez que han firmado [1][3].
La comunicación y la revocación destacan aún más diferencias. Imagina recibir una notificación a través de un portal de consentimiento dinámico sobre una nueva solicitud de datos. Puedes aprobar o revocar permisos para esa solicitud específica instantáneamente y recibir confirmación inmediata. Los métodos de consentimiento tradicional, sin embargo, podrían requerir que envíes formularios por correo o contactes directamente a los investigadores, llevando a retrasos e inconveniencias innecesarias [2][3][4].
Ambos modelos apuntan a alinearse con regulaciones como HIPAA y GDPR, pero los sistemas de consentimiento dinámico tienen una clara ventaja. Sus auditorías integradas y registros en tiempo real simplifican el cumplimiento con estándares de privacidad en evolución [2][5].
Cuándo Usar el Consentimiento Dinámico en la Compartición de Datos de Salud
Consentimiento Dinámico en Aplicaciones de Salud Impulsadas por IA
Las aplicaciones de salud impulsadas por IA prosperan en flujos de datos en tiempo real, lo que las hace un complemento perfecto para el consentimiento dinámico. Estas aplicaciones analizan diversas fuentes de datos - como dispositivos portátiles, biometría, pruebas de sangre y hábitos de vida - para proporcionar asesorías de salud personalizadas. El consentimiento estático a menudo no cumple en tales escenarios, ya que no puede seguir el ritmo continuo y la naturaleza en evolución de estos flujos de datos.
Toma Healify (https://healify.ai), por ejemplo. Esta aplicación presenta un coach de salud de IA llamado Anna, quien ofrece recomendaciones personalizadas las 24 horas del día procesando múltiples entradas de datos. Los usuarios reciben alertas en tiempo real como "PICO DE CORTISOL DETECTADO" o "BAJO NIVEL DE OXÍGENO EN SANGRE", personalizadas a su estado de salud actual. Con consentimiento dinámico, los usuarios pueden ajustar sus preferencias de intercambio de datos - por ejemplo, permitir el acceso a datos de sueño para consejos de manejo del estrés mientras se retienen los datos de pruebas de sangre. Este control granular no solo fomenta la confianza sino también garantiza el cumplimiento con regulaciones como HIPAA y GDPR, sostenido por auditorías en tiempo real.
El consentimiento dinámico también empodera a los usuarios para ajustar sus permisos de forma sencilla a través de un panel digital. Ya sea que cambien sus objetivos de salud o sus niveles de comodidad, pueden modificar configuraciones sin la molestia de firmar nuevos acuerdos. Este proceso optimizado mantiene a los usuarios en control mientras ofrece una experiencia fluida. Más allá de las aplicaciones de salud individuales, este enfoque sienta las bases para aplicaciones más amplias en el intercambio de datos de salud.
Mejores Casos de Uso para el Consentimiento Dinámico
El consentimiento dinámico demuestra su valía en escenarios donde el uso de datos evoluciona con el tiempo, como la investigación a largo plazo y las integraciones de dispositivos portátiles. Para los estudios longitudinales, es particularmente efectivo. Un gran ejemplo es el estudio Cooperativa de Investigación en Salud en Tirol del Sur (CHRIS), que comenzó en 2014 e involucró a 13,000 participantes. Usando una plataforma de consentimiento dinámico, los participantes pudieron actualizar sus preferencias y mantenerse informados sobre el acceso a datos durante una década [1]. Este enfoque no solo mantuvo el compromiso sino que también aseguró que los participantes se sintieran en control a lo largo del estudio.
Los dispositivos portátiles y la monitorización de salud en tiempo real también se benefician enormemente del consentimiento dinámico. Imagina tu reloj inteligente rastreando tu ritmo cardíaco, niveles de actividad, y patrones de sueño. Con el consentimiento dinámico, puedes pausar o ajustar el intercambio de datos conforme cambie tu nivel de comodidad - por ejemplo, restringiendo temporalmente los datos biométricos durante un período de estrés - sin detener toda la recolección de datos. Aplicaciones como Healify hacen esto posible, reduciendo la fatiga del consentimiento mientras mantienen a los usuarios involucrados activamente en la gestión de su salud.
La adaptabilidad del consentimiento dinámico lo convierte en una herramienta valiosa tanto en aplicaciones de salud personalizadas como en investigación a largo plazo, enfatizando el control y el compromiso centrado en el usuario.
Conclusión: Elegir el Modelo de Consentimiento Correcto
El consentimiento tradicional funciona bien para interacciones clínicas a corto plazo con un uso de datos sencillo. Se basa en formularios simples y estáticos y requiere pocos recursos técnicos, haciendo que sea una opción práctica para clínicas más pequeñas con presupuestos ajustados o para pacientes menos cómodos con herramientas digitales. Sin embargo, a medida que los ecosistemas de salud digitales se expanden y el uso de datos se vuelve más complejo, podría ser necesario un enfoque diferente.
Ahí es donde entra el consentimiento dinámico. Con su interfaz digital, el consentimiento dinámico permite a los usuarios tener un control continuo y detallado sobre sus datos. Los pacientes pueden modificar, retirar o volver a consentir usos específicos de datos a lo largo del tiempo. Esta interacción continua fomenta una mayor transparencia, confianza y compromiso en comparación con un proceso de consentimiento estático y único. Para plataformas impulsadas por IA como Healify, que recopilan datos de dispositivos portátiles, biometría, resultados de laboratorio y hábitos de vida, el consentimiento dinámico se alinea perfectamente con la manera en que los usuarios interactúan con su información de salud.
El modelo de consentimiento adecuado depende de tus necesidades de datos y capacidades organizacionales. Si gestionas grandes volúmenes de datos sensibles de múltiples fuentes, el consentimiento dinámico es más adecuado para acomodar la complejidad y reflejar las preferencias del paciente. Las organizaciones con sistemas de TI avanzados y un enfoque en la participación del paciente encontrarán el consentimiento dinámico particularmente beneficioso.
Para las organizaciones de atención médica de EE. UU., varios factores deberían influir en esta decisión: requisitos regulatorios, volumen y sensibilidad de los datos, la alfabetización digital de la población a la que se sirve, la infraestructura técnica y el presupuesto. Implementar el consentimiento dinámico requiere inversiones en plataformas digitales seguras, integración con registros de salud electrónicos, y actualizaciones en tiempo real para asegurar que las elecciones de los pacientes sean respetadas. Sin embargo, también es crucial abordar las barreras potenciales, como excluir a pacientes con acceso digital limitado o menor alfabetización tecnológica.
En EE. UU., donde los datos de dispositivos portátiles y resultados de laboratorio alimentan cada vez más modelos de IA, el consentimiento dinámico asegura que la personalización respete la autonomía y privacidad del paciente. Como se muestra en la tabla de comparación, el consentimiento dinámico ofrece la flexibilidad y transparencia necesarias para la gestión moderna de datos de salud. Esta elección no solo respalda el cumplimiento regulatorio sino que también fortalece la confianza del paciente, elementos clave de un consentimiento efectivo y centrado en el paciente en el panorama digital de salud actual.
Preguntas Frecuentes
¿Qué hace que el consentimiento dinámico sea más empoderador para los pacientes en comparación con el consentimiento tradicional?
El consentimiento dinámico pone a los pacientes en el asiento del conductor cuando se trata de sus datos de salud. A diferencia del enfoque tradicional único para el consentimiento, este modelo permite a las personas gestionar continuamente sus preferencias. Ya sea que deseen actualizar, ajustar o incluso revocar sus decisiones, el consentimiento dinámico los mantiene activamente involucrados en decidir cómo se usan sus datos.
Esta adaptabilidad en tiempo real lo convierte en una forma más personalizada y receptiva de manejar datos de salud. Al alinearse con las necesidades y prioridades cambiantes de las personas, construye una base más fuerte de confianza y apertura entre los pacientes y quienes gestionan su información.
¿Qué necesitan los sistemas de salud para implementar el consentimiento dinámico?
Para hacer del consentimiento dinámico una realidad, los sistemas de salud necesitan una configuración de gestión de datos confiable y adaptable capaz de manejar actualizaciones en tiempo real de preferencias de consentimiento. Esta configuración debe incluir medidas de autenticación fuertes, adherirse a leyes de privacidad como HIPAA, y conectarse sin problemas con registros de salud electrónicos (EHRs) para monitorear y gestionar el consentimiento de manera efectiva.
Igual de importante es una interfaz simple e intuitiva que empodere a los individuos para ajustar sus preferencias de consentimiento cuando sea necesario. Asegurar que los sistemas puedan trabajar juntos de manera fluida también es clave para compartir datos de manera eficiente mientras se respetan la privacidad y los límites de consentimiento.
¿Puede el consentimiento dinámico funcionar con los sistemas actuales de registros de salud electrónicos?
Sí, el consentimiento dinámico puede funcionar sin problemas con los sistemas existentes de registros de salud electrónicos (EHRs). Su marco adaptable se ajusta a varias plataformas de gestión de datos de salud, mejorando la forma en que se rastrean y gestionan las preferencias de los pacientes.
Al integrar el consentimiento dinámico, los proveedores de salud pueden simplificar los procedimientos de consentimiento, otorgando a los pacientes más control sobre sus datos de salud mientras alinean con las regulaciones de privacidad.
Publicaciones del Blog Relacionadas
El consentimiento es la forma en que controlas quién usa tus datos de salud y con qué propósito. El consentimiento dinámico te ofrece un control continuo a través de herramientas digitales, mientras que el consentimiento tradicional es un acuerdo único con flexibilidad limitada. Aquí tienes un resumen rápido:
Consentimiento Dinámico: Te permite actualizar permisos en cualquier momento a través de una plataforma segura. Puedes gestionar usos específicos de datos, retirar selectivamente los permisos y hacer un seguimiento de quién accede a tus datos.
Consentimiento Tradicional: Implica la firma de un formulario amplio y estático. Los cambios requieren la retirada completa, y rara vez ves cómo se utilizan tus datos.
El consentimiento dinámico es ideal para aplicaciones de salud modernas y estudios a largo plazo donde el uso de datos evoluciona, mientras que el consentimiento tradicional funciona para necesidades más simples y a corto plazo.
Comparación Rápida
Característica | Consentimiento Dinámico | Consentimiento Tradicional |
|---|---|---|
Flexibilidad | Alta: Actualiza permisos en cualquier momento | Baja: Acuerdo único |
Control | Completo: Gestiona usos específicos de datos | Limitado: Permisos amplios y generales |
Transparencia | Alta: Acceso a registros y notificaciones | Baja: Visibilidad mínima tras la firma |
Revocación | Fácil: Retira permisos específicos | Difícil: Requiere retirada completa |
Mejores Casos de Uso | Aplicaciones de IA, dispositivos portátiles, estudios a largo plazo | Estudios a corto plazo, necesidades de datos simples |
El consentimiento dinámico se alinea con los sistemas de salud digital actuales, ofreciendo más control y transparencia. El consentimiento tradicional es más simple pero menos adecuado para un uso de datos en evolución.
Consentimiento Dinámico vs Consentimiento Tradicional: Tabla de Comparación de Características
Consentimiento Dinámico
¿Qué es el Consentimiento Tradicional?
El consentimiento tradicional es un acuerdo fijo, único donde las personas otorgan un permiso amplio para el uso de sus datos de salud, a menudo con una sola firma.
Características del Consentimiento Tradicional
En este modelo, los pacientes firman formularios que permiten el acceso a sus biospecímenes y registros de salud para propósitos futuros no especificados. Normalmente, este proceso se basa en métodos en papel o sistemas electrónicos básicos. Sin embargo, carece de la flexibilidad para ajustarse a objetivos de investigación en evolución o nuevos usos para los datos [1].
Fortalezas del Consentimiento Tradicional
La simplicidad del consentimiento tradicional lo hace fácil de implementar y ampliamente accesible. El proceso es directo: los participantes leen un formulario, lo firman, y su participación está confirmada. Esta simplicidad se traduce en menores costos para las organizaciones y asegura accesibilidad para individuos que pueden no usar plataformas digitales. Históricamente, los formularios de consentimiento en papel fueron el método preferido para biobancos y ensayos clínicos antes de que los modelos de consentimiento dinámico estuvieran disponibles [1].
Limitaciones del Consentimiento Tradicional
Una de las mayores desventajas del consentimiento tradicional es su rigidez. Los participantes que se sientan incómodos con ciertos aspectos de un estudio deben retirarse por completo, ya que el modelo no permite ajustes selectivos a los permisos. Una vez dado el consentimiento, no hay forma de actualizar preferencias o revocar permisos específicos sin abandonar el estudio por completo. Este enfoque todo-o-nada puede desalentar la participación continua y puede no respetar completamente la autonomía del participante a medida que la investigación evoluciona.
Además, el consentimiento tradicional no se alinea bien con los sistemas digitales modernos, como aplicaciones de salud impulsadas por IA o dispositivos portátiles que recopilan datos continuamente. Estas tecnologías requieren permisos más detallados y auditorías más robustas para cumplir con regulaciones como HIPAA y GDPR [1]. Esta falta de adaptabilidad ha dado paso a modelos de consentimiento dinámico, que proporcionan opciones más flexibles y continuas para los participantes.
¿Qué es el Consentimiento Dinámico?
El consentimiento dinámico es una forma moderna e interactiva de gestionar cómo se usa tu información de salud. En lugar de firmar un formulario de consentimiento único que cubra todos los posibles usos, este enfoque te ofrece un control continuo. A través de una plataforma digital segura, puedes actualizar tus preferencias en cualquier momento, adaptando los permisos a medida que tu nivel de comodidad o circunstancias evolucionan.
Este sistema prioriza la comunicación en tiempo real entre tú y las organizaciones que usan tus datos. Te permite decidir, en detalle, quién puede acceder a tu información, qué datos pueden usar, y con qué propósitos - todo con la capacidad de ajustar estas configuraciones instantáneamente.
Características Clave del Consentimiento Dinámico
Una de las características destacadas del consentimiento dinámico es su panel de usuario amigable. Este panel muestra tus permisos actuales y te permite optar por o en contra con un solo clic. Cualquier cambio que realices se aplica inmediatamente en todos los sistemas que gestionan tus datos.
El sistema también ofrece un control detallado sobre tus permisos. Por ejemplo, puedes especificar el consentimiento basado en el tipo de datos - ya sea información genómica, datos de dispositivos portátiles, o registros de salud mental. También puedes definir permisos basados en el propósito, como si los datos se usarán para coaching personal, investigación, o fines comerciales, e incluso establecer límites de tiempo para cuánto tiempo se pueden usar tus datos. Para ayudarte a mantenerte informado, la plataforma proporciona notificaciones y recursos educativos sobre nuevos usos de datos.
Tras bambalinas, el sistema mantiene un registro en tiempo real de eventos de acceso a datos y cambios de consentimiento. Estas auditorías aseguran el cumplimiento con regulaciones de privacidad como HIPAA y construyen confianza al documentar cómo se maneja tu información.
Beneficios del Consentimiento Dinámico
El consentimiento dinámico te pone a cargo de tus datos de salud, permitiéndote ajustar permisos sin el enfoque todo-o-nada de los modelos tradicionales. Puedes retirar permisos específicos sin detener todo el intercambio de datos, lo que ayuda a combatir la "fatiga del consentimiento" centralizando todo en un solo lugar.
El formato digital también facilita la comprensión de a qué estás accediendo. Visuales claros y explicaciones sencillas te ayudan a revisar y ajustar configuraciones rápidamente. Para las organizaciones, este enfoque no solo asegura el cumplimiento con las leyes de privacidad, sino que también apoya estudios a largo plazo al mantener a los participantes comprometidos y sintiéndose en control.
Al ofrecer este nivel de flexibilidad y transparencia, el consentimiento dinámico fortalece la confianza y mejora la relación entre los usuarios y las plataformas de salud digital.
Ejemplos de Uso de Consentimiento Dinámico
El consentimiento dinámico ya está causando impacto en la salud digital. Por ejemplo, aplicaciones impulsadas por IA que analizan datos de dispositivos portátiles, biometría, pruebas de sangre y hábitos de vida pueden usar este modelo para darte control completo sobre qué flujos de datos se comparten. Imagina una plataforma como Healify, donde puedes otorgar o revocar acceso a fuentes de datos específicas, como el ritmo cardíaco de tu reloj inteligente, tus patrones de sueño o resultados de laboratorio. También podrías decidir si tus datos desidentificados se usan exclusivamente para coaching personal o si pueden contribuir al desarrollo de algoritmos e investigación.
Este nivel de control garantiza que tus datos se usen de formas que se alinean con tus preferencias, convirtiendo al consentimiento dinámico en un cambio radical en la gestión de salud personalizada.
Diferencias Clave entre el Consentimiento Dinámico y el Tradicional
Tabla de Comparación: Consentimiento Dinámico vs. Consentimiento Tradicional
Cuando comparas el consentimiento dinámico y el tradicional lado a lado, las diferencias son notables. El consentimiento tradicional se basa en un formulario único, a menudo redactado en términos generales, que cubre todos los usos futuros de tus datos y es difícil de modificar. Sin embargo, el consentimiento dinámico ofrece control continuo a través de herramientas digitales, facilitando el ajuste de permisos cuando sea necesario.
Atributo | Consentimiento Dinámico | Consentimiento Tradicional |
|---|---|---|
Flexibilidad | Alta: Actualizaciones en tiempo real con permisos específicos para tipos de datos y plazos | Baja: Formularios estáticos que requieren nueva documentación para cambios |
Control de Participantes | Completo: Paneles digitales te permiten gestionar permisos para usos de datos individuales | Limitado: Permisos amplios y generales con mínima intervención del participante después de firmar |
Comunicación | Interacción continua y bidireccional a través de plataformas seguras con actualizaciones y notificaciones | Conversación única o formulario al inicio |
Revocación | Inmediata y parcial: Retira permisos específicos sin dejar el estudio | Consumo de tiempo y a menudo requiere retirada completa a través de documentación extensa |
Transparencia | Alta: Auditorías detalladas muestran quién accedió a tus datos, cuándo y por qué | Baja: Visibilidad limitada al uso de datos después del primer consentimiento |
Estas diferencias se vuelven más claras al explorarlas a través de escenarios del mundo real.
Comprendiendo las Diferencias con Ejemplos
Toma como ejemplo la investigación de salud a largo plazo. Con el consentimiento dinámico, los participantes pueden ajustar sus permisos con el tiempo. Por ejemplo, alguien podría permitir el uso de sus registros de salud para un estudio específico hoy pero decidir restringir el acceso a ciertos tipos de datos en el futuro. En cambio, el consentimiento tradicional bloquea a los participantes en un acuerdo "todo-o-nada", ofreciendo ninguna flexibilidad para refinar sus elecciones más tarde.
El control del participante es otra diferencia clave. Las plataformas de consentimiento dinámico empoderan a los usuarios para tomar decisiones precisas, como aprobar el uso de datos biométricos pero declinar el uso de información genética. Estas plataformas también proporcionan registros de acceso para que los participantes puedan ver exactamente cómo se utilizan sus datos. Por otro lado, los formularios de consentimiento tradicional a menudo utilizan un lenguaje vago, dejando a los participantes con poca información o control una vez que han firmado [1][3].
La comunicación y la revocación destacan aún más diferencias. Imagina recibir una notificación a través de un portal de consentimiento dinámico sobre una nueva solicitud de datos. Puedes aprobar o revocar permisos para esa solicitud específica instantáneamente y recibir confirmación inmediata. Los métodos de consentimiento tradicional, sin embargo, podrían requerir que envíes formularios por correo o contactes directamente a los investigadores, llevando a retrasos e inconveniencias innecesarias [2][3][4].
Ambos modelos apuntan a alinearse con regulaciones como HIPAA y GDPR, pero los sistemas de consentimiento dinámico tienen una clara ventaja. Sus auditorías integradas y registros en tiempo real simplifican el cumplimiento con estándares de privacidad en evolución [2][5].
Cuándo Usar el Consentimiento Dinámico en la Compartición de Datos de Salud
Consentimiento Dinámico en Aplicaciones de Salud Impulsadas por IA
Las aplicaciones de salud impulsadas por IA prosperan en flujos de datos en tiempo real, lo que las hace un complemento perfecto para el consentimiento dinámico. Estas aplicaciones analizan diversas fuentes de datos - como dispositivos portátiles, biometría, pruebas de sangre y hábitos de vida - para proporcionar asesorías de salud personalizadas. El consentimiento estático a menudo no cumple en tales escenarios, ya que no puede seguir el ritmo continuo y la naturaleza en evolución de estos flujos de datos.
Toma Healify (https://healify.ai), por ejemplo. Esta aplicación presenta un coach de salud de IA llamado Anna, quien ofrece recomendaciones personalizadas las 24 horas del día procesando múltiples entradas de datos. Los usuarios reciben alertas en tiempo real como "PICO DE CORTISOL DETECTADO" o "BAJO NIVEL DE OXÍGENO EN SANGRE", personalizadas a su estado de salud actual. Con consentimiento dinámico, los usuarios pueden ajustar sus preferencias de intercambio de datos - por ejemplo, permitir el acceso a datos de sueño para consejos de manejo del estrés mientras se retienen los datos de pruebas de sangre. Este control granular no solo fomenta la confianza sino también garantiza el cumplimiento con regulaciones como HIPAA y GDPR, sostenido por auditorías en tiempo real.
El consentimiento dinámico también empodera a los usuarios para ajustar sus permisos de forma sencilla a través de un panel digital. Ya sea que cambien sus objetivos de salud o sus niveles de comodidad, pueden modificar configuraciones sin la molestia de firmar nuevos acuerdos. Este proceso optimizado mantiene a los usuarios en control mientras ofrece una experiencia fluida. Más allá de las aplicaciones de salud individuales, este enfoque sienta las bases para aplicaciones más amplias en el intercambio de datos de salud.
Mejores Casos de Uso para el Consentimiento Dinámico
El consentimiento dinámico demuestra su valía en escenarios donde el uso de datos evoluciona con el tiempo, como la investigación a largo plazo y las integraciones de dispositivos portátiles. Para los estudios longitudinales, es particularmente efectivo. Un gran ejemplo es el estudio Cooperativa de Investigación en Salud en Tirol del Sur (CHRIS), que comenzó en 2014 e involucró a 13,000 participantes. Usando una plataforma de consentimiento dinámico, los participantes pudieron actualizar sus preferencias y mantenerse informados sobre el acceso a datos durante una década [1]. Este enfoque no solo mantuvo el compromiso sino que también aseguró que los participantes se sintieran en control a lo largo del estudio.
Los dispositivos portátiles y la monitorización de salud en tiempo real también se benefician enormemente del consentimiento dinámico. Imagina tu reloj inteligente rastreando tu ritmo cardíaco, niveles de actividad, y patrones de sueño. Con el consentimiento dinámico, puedes pausar o ajustar el intercambio de datos conforme cambie tu nivel de comodidad - por ejemplo, restringiendo temporalmente los datos biométricos durante un período de estrés - sin detener toda la recolección de datos. Aplicaciones como Healify hacen esto posible, reduciendo la fatiga del consentimiento mientras mantienen a los usuarios involucrados activamente en la gestión de su salud.
La adaptabilidad del consentimiento dinámico lo convierte en una herramienta valiosa tanto en aplicaciones de salud personalizadas como en investigación a largo plazo, enfatizando el control y el compromiso centrado en el usuario.
Conclusión: Elegir el Modelo de Consentimiento Correcto
El consentimiento tradicional funciona bien para interacciones clínicas a corto plazo con un uso de datos sencillo. Se basa en formularios simples y estáticos y requiere pocos recursos técnicos, haciendo que sea una opción práctica para clínicas más pequeñas con presupuestos ajustados o para pacientes menos cómodos con herramientas digitales. Sin embargo, a medida que los ecosistemas de salud digitales se expanden y el uso de datos se vuelve más complejo, podría ser necesario un enfoque diferente.
Ahí es donde entra el consentimiento dinámico. Con su interfaz digital, el consentimiento dinámico permite a los usuarios tener un control continuo y detallado sobre sus datos. Los pacientes pueden modificar, retirar o volver a consentir usos específicos de datos a lo largo del tiempo. Esta interacción continua fomenta una mayor transparencia, confianza y compromiso en comparación con un proceso de consentimiento estático y único. Para plataformas impulsadas por IA como Healify, que recopilan datos de dispositivos portátiles, biometría, resultados de laboratorio y hábitos de vida, el consentimiento dinámico se alinea perfectamente con la manera en que los usuarios interactúan con su información de salud.
El modelo de consentimiento adecuado depende de tus necesidades de datos y capacidades organizacionales. Si gestionas grandes volúmenes de datos sensibles de múltiples fuentes, el consentimiento dinámico es más adecuado para acomodar la complejidad y reflejar las preferencias del paciente. Las organizaciones con sistemas de TI avanzados y un enfoque en la participación del paciente encontrarán el consentimiento dinámico particularmente beneficioso.
Para las organizaciones de atención médica de EE. UU., varios factores deberían influir en esta decisión: requisitos regulatorios, volumen y sensibilidad de los datos, la alfabetización digital de la población a la que se sirve, la infraestructura técnica y el presupuesto. Implementar el consentimiento dinámico requiere inversiones en plataformas digitales seguras, integración con registros de salud electrónicos, y actualizaciones en tiempo real para asegurar que las elecciones de los pacientes sean respetadas. Sin embargo, también es crucial abordar las barreras potenciales, como excluir a pacientes con acceso digital limitado o menor alfabetización tecnológica.
En EE. UU., donde los datos de dispositivos portátiles y resultados de laboratorio alimentan cada vez más modelos de IA, el consentimiento dinámico asegura que la personalización respete la autonomía y privacidad del paciente. Como se muestra en la tabla de comparación, el consentimiento dinámico ofrece la flexibilidad y transparencia necesarias para la gestión moderna de datos de salud. Esta elección no solo respalda el cumplimiento regulatorio sino que también fortalece la confianza del paciente, elementos clave de un consentimiento efectivo y centrado en el paciente en el panorama digital de salud actual.
Preguntas Frecuentes
¿Qué hace que el consentimiento dinámico sea más empoderador para los pacientes en comparación con el consentimiento tradicional?
El consentimiento dinámico pone a los pacientes en el asiento del conductor cuando se trata de sus datos de salud. A diferencia del enfoque tradicional único para el consentimiento, este modelo permite a las personas gestionar continuamente sus preferencias. Ya sea que deseen actualizar, ajustar o incluso revocar sus decisiones, el consentimiento dinámico los mantiene activamente involucrados en decidir cómo se usan sus datos.
Esta adaptabilidad en tiempo real lo convierte en una forma más personalizada y receptiva de manejar datos de salud. Al alinearse con las necesidades y prioridades cambiantes de las personas, construye una base más fuerte de confianza y apertura entre los pacientes y quienes gestionan su información.
¿Qué necesitan los sistemas de salud para implementar el consentimiento dinámico?
Para hacer del consentimiento dinámico una realidad, los sistemas de salud necesitan una configuración de gestión de datos confiable y adaptable capaz de manejar actualizaciones en tiempo real de preferencias de consentimiento. Esta configuración debe incluir medidas de autenticación fuertes, adherirse a leyes de privacidad como HIPAA, y conectarse sin problemas con registros de salud electrónicos (EHRs) para monitorear y gestionar el consentimiento de manera efectiva.
Igual de importante es una interfaz simple e intuitiva que empodere a los individuos para ajustar sus preferencias de consentimiento cuando sea necesario. Asegurar que los sistemas puedan trabajar juntos de manera fluida también es clave para compartir datos de manera eficiente mientras se respetan la privacidad y los límites de consentimiento.
¿Puede el consentimiento dinámico funcionar con los sistemas actuales de registros de salud electrónicos?
Sí, el consentimiento dinámico puede funcionar sin problemas con los sistemas existentes de registros de salud electrónicos (EHRs). Su marco adaptable se ajusta a varias plataformas de gestión de datos de salud, mejorando la forma en que se rastrean y gestionan las preferencias de los pacientes.
Al integrar el consentimiento dinámico, los proveedores de salud pueden simplificar los procedimientos de consentimiento, otorgando a los pacientes más control sobre sus datos de salud mientras alinean con las regulaciones de privacidad.
Publicaciones del Blog Relacionadas
Finalmente toma el control de tu salud

Finalmente toma el control de tu salud

Finalmente toma el control de tu salud





