Improve your health
Improve your health
Improve your health
January 6, 2026
How AI Wearables Improve Cancer Patient Outcomes


AI-powered wearables are transforming cancer care by providing continuous, real-time health monitoring. Unlike periodic clinic visits, these devices track metrics like heart rate, sleep patterns, and physical activity around the clock. This allows doctors to detect early warning signs, tailor treatments, and improve patient adherence to care plans. Key findings include:
Continuous Monitoring: Devices collect 24/7 data, offering a clearer picture of patient health compared to intermittent checkups.
Improved Outcomes: Studies show increasing daily steps by 1,000 can reduce death risk by 52% and hospitalizations by 79%.
Personalized Care: AI analyzes patterns to create individual health profiles, enabling timely interventions.
Treatment Support: Wearables enhance medication adherence and physical activity through real-time coaching.
Despite challenges like data privacy and accessibility, these tools are reshaping cancer care by providing actionable insights that improve patient outcomes.
How Wearables Are Transforming Oncology Care
1. AI Wearables
AI-powered wearables are reshaping how oncologists monitor cancer patients by providing continuous, real-world data. Unlike traditional methods that depend on clinic visits every few weeks, these devices track vital metrics like heart rate, body temperature, oxygen levels (SpO2), and physical activity 24/7. The data is uploaded to the cloud within minutes, giving clinicians almost immediate access to patient health updates [8].
Real-Time Monitoring
One of the standout features of AI wearables is their ability to collect and analyze digital biomarkers - physiological signals that reveal a patient’s condition and symptom burden [3]. A report from Memorial Sloan Kettering Cancer Center, published in October 2024, showcased how three lung cancer patients (ages 55–71) were monitored using Apple Health data. Over 58 to 135 weeks, the system gathered between 34,319 and 103,535 physiological data points per patient, averaging around 41 measures daily. This continuous monitoring revealed changes in health that traditional ECOG scores might have missed.
AI algorithms excel at detecting anomalies, often identifying potential problems before patients even notice symptoms [3]. For instance, machine learning models using smartwatch data have achieved up to 93% accuracy in predicting mortality for end-of-life cancer patients [10]. These insights pave the way for more personalized care and better treatment management.
Treatment Adherence
AI wearables also play a key role in improving treatment adherence by offering personalized coaching and real-time feedback. Take the CAPRI trial, for example. This study involved 559 patients on oral anticancer medications and paired a nurse-led program with a smartphone app. Patients in the intervention group maintained a 93.4% relative dose intensity compared to 89.4% in the usual care group. They also experienced fewer severe toxicities and spent less time in the hospital [12].
"Patient-centered care through remote monitoring of symptoms and treatment may improve patient outcomes and experience." – Olivier Mir, Department of Ambulatory Cancer Care, Gustave Roussy [12]
Another study, the PATH trial at Johns Hopkins University, highlighted the impact of AI-guided interventions. In this trial, 42 overweight or sedentary cancer survivors used the AI voice-assisted "MyCoach" system, which integrated Fitbit Charge 2 HR data. Over four weeks, participants in the MyCoach group increased their daily step count by 3,568.9 steps (P < 0.001), compared to an increase of only 1,619 steps with basic text messaging. The system’s ability to provide personalized, two-way interaction significantly boosted adherence to physical activity [4].
Personalization
AI wearables don’t just track data - they use it to create highly individualized care plans. By analyzing patterns in sleep, activity, and medication adherence, these devices build a detailed health profile for each patient. This allows for timely, targeted interventions tailored to the individual’s needs [3][4].
"Wearable devices hold significant promise for the development of personalized 'digital biomarkers,' which may enhance risk stratification and management in oncology." – Joshua W. Bliss, New York Presbyterian, Weill Cornell Medicine [6]
Early Detection
The ability to detect subtle changes early is another major advantage of AI wearables. In the bwHealthApp pilot study, 31 gastrointestinal cancer outpatients at University Hospital Tübingen used wrist and in-ear devices between July and October 2022. These wearables collected over 20 million data points, including heart rate and temperature, in near real-time [8]. With this wealth of information, clinicians identified subtle physiological shifts that signaled potential hospitalizations or disease progression - issues that might have been overlooked during routine checkups. Additionally, a review of 199 studies found that more than 74% of patients adhered to wearable devices, showcasing their practicality [9].
At Healify, we’re taking this further by transforming wearable data into actionable insights. Our AI health coach, Anna, offers 24/7 personalized guidance, ensuring each patient gets support tailored to their unique health profile.
2. Standard Monitoring Methods
In traditional cancer care, patient progress is typically tracked through scheduled clinic visits. These appointments occur at set intervals during and after treatment [6]. At each visit, healthcare providers assess patients using subjective tools like the ECOG Performance Status and the Karnofsky Performance Status (KPS) to determine how well they can manage daily activities. They also analyze blood tests, imaging results, and cardiac evaluations to gauge overall health [6].
Real-Time Monitoring
The standard approach provides only periodic glimpses into a patient’s condition due to the infrequency of clinic visits [7]. Between these appointments, doctors rely heavily on patients' recollection of symptoms - a method often affected by recall bias. For instance, a study on advanced cancer patients revealed that those with a poor ECOG status (ECOG 3) averaged just 902 steps per day, compared to 5,345 steps for patients with a better ECOG status of 0 [7].
"Low sampling frequency due to periodic intervals of in-person visits during the treatment course further limits monitoring. Failure to detect early physiological symptoms contributes to suboptimal therapeutic management and poor clinical outcomes." – Frontiers in Oncology [6]
These constraints highlight the need for continuous, data-driven monitoring systems.
Treatment Adherence and Personalization
Tracking whether patients stick to their treatment plans is another challenge for standard monitoring methods. Relying on patients to recall and report their symptoms during visits often leads to underestimating symptom severity [3]. Additionally, static evaluations conducted before treatment fail to account for daily variations in a patient’s health, making it difficult to tailor care to their changing needs [6][7].
Early Detection
Traditional methods often miss critical early warning signs. A study conducted in October 2025 by researchers at Northwell Health's Feinstein Institutes examined 888 adult non-ICU inpatients. The findings showed that AI-powered continuous monitoring could predict patient deterioration an average of 17 hours earlier than standard intermittent vital sign checks. The AI system identified 83% of unplanned ICU transfers and successfully detected all cases of cardiac arrest or death within 24 hours [17].
"Currently, hospital staff rely on intermittent vital sign checks of a patient, like their heart rate or temperature, to identify worsening conditions. Combining clinical wearables with the predictive AI algorithm we have developed, we can help clinicians identify these deteriorations a lot earlier and more accurately than standard-of-care early warning scores." – Theodoros P. Zanos, PhD, Head of Northwell's Division of Health AI [17]
This inability to catch early signs of deterioration underscores the advantages of AI-driven wearables in providing timely and accurate patient insights.
Advantages and Disadvantages
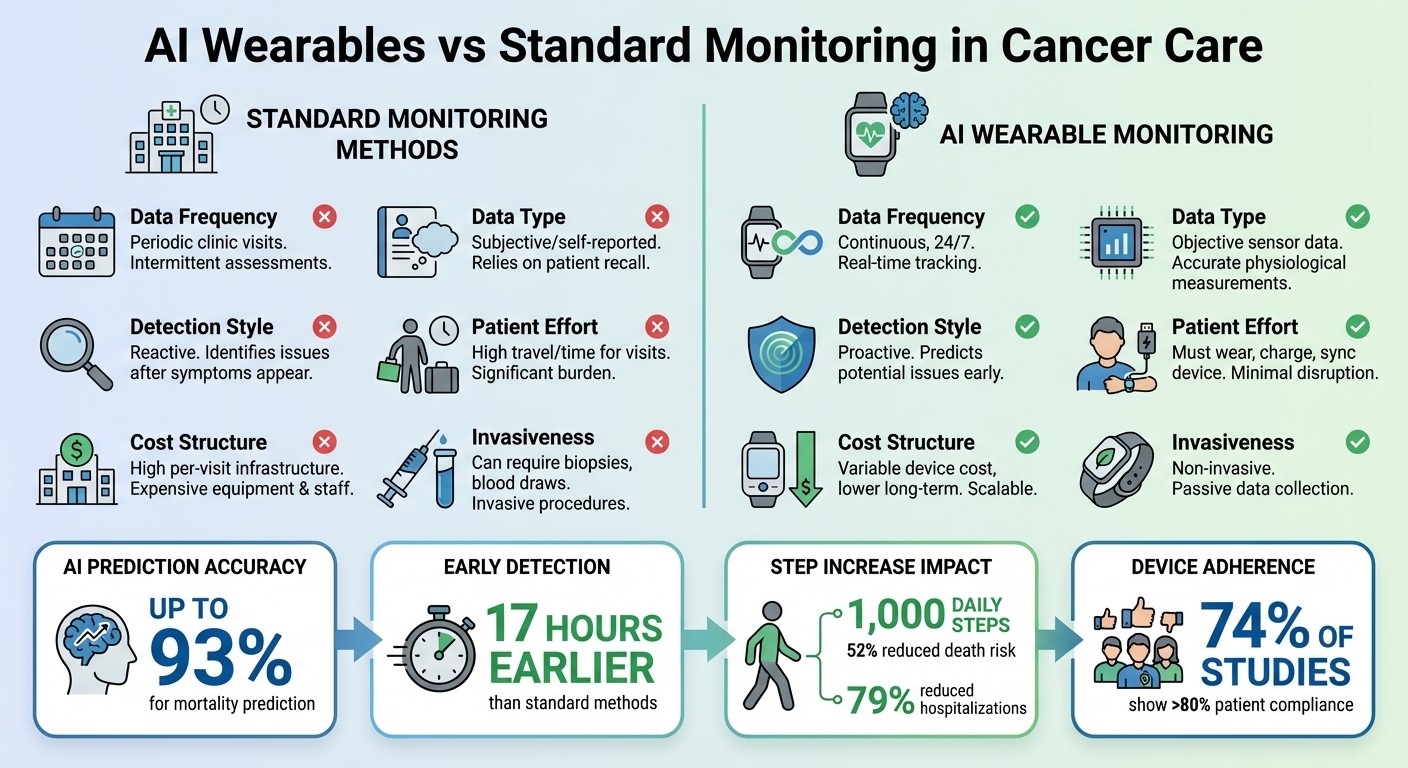
AI Wearables vs Standard Monitoring Methods in Cancer Care
When you stack AI wearables against traditional monitoring methods, the differences are striking. AI-driven devices provide round-the-clock data, while conventional methods depend on periodic snapshots during clinic visits. Wearables collect objective physiological data like heart rate variability and step counts, whereas traditional approaches often rely on self-reported information that can be skewed by memory lapses or biases [2]. This comparison shows how AI wearables address the gaps in accuracy and consistency seen in older methods.
AI systems also excel at predicting clinical outcomes. For instance, machine learning models have demonstrated impressive accuracy rates - up to 93% when analyzing medical images and 89% with smartwatch data [1][10]. In one study, advanced cancer patients who increased their daily steps by just 1,000 saw a 0.34 odds ratio for adverse events and a 48% reduction in death risk (HR: 0.48) [7].
That said, these devices aren’t without their challenges. Data privacy is a major concern due to the sheer volume of sensitive information being collected, which demands secure storage and regulated sharing [5]. There are also technical hurdles - sensors can be thrown off by motion distortions or environmental noise, and step counts might be less accurate for individuals with slower gaits [2][5]. Another issue is the "black box" nature of many AI models, which can make their decision-making processes less transparent and harder for clinicians to trust [1][21].
Feature | Standard Monitoring | AI Wearable Monitoring |
|---|---|---|
Data Frequency | Periodic clinic visits [10] | Continuous, 24/7 [6] |
Data Type | Subjective/self-reported [2] | Objective sensor data [2] |
Detection Style | Reactive [10] | Proactive [5] |
Patient Effort | High travel/time for visits [10] | Must wear, charge, sync device [20] |
Cost Structure | High per-visit infrastructure [10] | Variable device cost, lower long-term [10] |
Invasiveness | Can require biopsies, blood draws [10] | Non-invasive [5] |
While AI wearables clearly bring a host of benefits, there are barriers to widespread adoption. Digital literacy and access to reliable internet connectivity are key factors. These technologies often favor populations with strong digital skills and access to smartphones, potentially leaving others behind [1]. Older adults, in particular, may lack the devices or home internet needed for these wearables to work effectively [2]. On a positive note, adherence to these devices is high: over 80% of participants in 74% of studies reported consistent usage [9].
Conclusion
AI wearables are reshaping the landscape of cancer care by providing continuous, real-time health data. These devices offer a dynamic view of a patient’s condition, enabling early detection of potential issues and timely medical intervention.
Take the PATH trial at Johns Hopkins University as an example. Led by Ahmed Hassoon, this study explored the integration of AI with wearable technology. Cancer survivors who used the AI voice coach "MyCoach" increased their daily physical activity by an average of 3,568.9 steps over four weeks. This improvement significantly outpaced the results seen in control groups.
"AI-based voice-assisted coaching shows promise as a practical method of delivering scalable, individualized coaching to increase physical activity in sedentary cancer survivors" [4].
The implications of wearable data go beyond step counts. By leveraging this information, healthcare providers can refine treatment plans, better assess frailty, and predict chemotherapy tolerance more effectively than with traditional methods. Features like monitoring step counts as a vital sign and receiving automated alerts when thresholds are exceeded enable clinicians to act proactively [3][5].
However, there’s a notable gap in adoption - only 29% of cancer survivors currently use wearable activity trackers. Bridging this digital divide requires addressing barriers like access to devices, reliable internet, and digital literacy [11].
Pulling all this together, AI wearables are becoming indispensable in cancer care. They enhance treatment adherence and empower patients with tailored insights into their health. Platforms like Healify take this a step further, translating complex wearable data into actionable advice, ensuring cancer patients receive continuous support throughout their journey.
FAQs
How do AI-powered wearables help cancer patients stick to their treatment plans?
AI-powered wearables take raw health data - like heart rate, activity levels, sleep patterns, and medication schedules - and turn it into meaningful insights tailored to each individual. These devices analyze the information to spot missed doses, worsening symptoms, or noticeable changes in health. When something seems off, they send real-time alerts and practical advice to patients. With permission, they can also notify care teams, allowing for quick and effective interventions.
These wearables go a step further by offering custom medication reminders, predicting times when patients might struggle with adherence (like after chemotherapy), and adjusting coaching prompts to help users stay on track. Research shows that patients using these devices are more likely to follow their treatment plans, keep better tabs on their symptoms, and engage more with recommended activities - all of which contribute to better health outcomes. By blending constant monitoring with personalized support, these tools help patients stick to their therapy plans and take control of their health.
What are the challenges of using AI wearables in cancer care?
AI-powered wearables hold promise for reshaping cancer care, but they come with their own set of hurdles. One major challenge is integrating data from consumer-grade devices into clinical workflows. Aligning this data with medical-grade standards and meeting regulatory requirements can be a tricky process. On top of that, the constant transmission of sensitive health data raises serious privacy and security concerns, including issues around consent, data storage, and the risk of breaches.
Patient adherence is another significant obstacle. While many cancer patients start using wearables, they often abandon them due to discomfort, short battery life, or a lack of noticeable benefits. Socioeconomic factors also play a role - affordability and digital literacy can limit access to these technologies, leaving some populations behind. Furthermore, AI algorithms may generate biased or inaccurate results if they’re trained on datasets that don’t reflect diverse populations, which could unintentionally deepen health disparities.
Platforms like Healify are stepping up to tackle these challenges. By securely analyzing wearable data, they deliver personalized, actionable insights to users. With an emphasis on user-friendly design, clinical validation, and robust data security, solutions like Healify aim to make AI wearables more practical and accessible for improving cancer care.
How do AI wearables help detect health issues early for cancer patients?
AI-powered wearables are transforming personal health monitoring by tracking key metrics like heart rate, blood pressure, oxygen levels, sleep patterns, and activity levels - all in real time. These devices use AI to compare this data against personalized baselines, spotting subtle changes that might indicate potential health concerns before symptoms even surface. For instance, wearables have been used to identify early signs of infections in chemotherapy patients, helping to prevent serious cancer-related complications.
Beyond just detecting irregularities, these devices provide actionable alerts for both patients and their healthcare teams. Whether it's a warning about arrhythmias or early indicators of sepsis, these notifications can lead to timely interventions, ultimately reducing hospital visits and improving patient outcomes. Platforms such as Healify take this a step further by combining wearable data with health records and lifestyle information. This creates a 24/7 stream of personalized health insights, empowering patients and clinicians to address potential issues proactively.
Related Blog Posts
AI-powered wearables are transforming cancer care by providing continuous, real-time health monitoring. Unlike periodic clinic visits, these devices track metrics like heart rate, sleep patterns, and physical activity around the clock. This allows doctors to detect early warning signs, tailor treatments, and improve patient adherence to care plans. Key findings include:
Continuous Monitoring: Devices collect 24/7 data, offering a clearer picture of patient health compared to intermittent checkups.
Improved Outcomes: Studies show increasing daily steps by 1,000 can reduce death risk by 52% and hospitalizations by 79%.
Personalized Care: AI analyzes patterns to create individual health profiles, enabling timely interventions.
Treatment Support: Wearables enhance medication adherence and physical activity through real-time coaching.
Despite challenges like data privacy and accessibility, these tools are reshaping cancer care by providing actionable insights that improve patient outcomes.
How Wearables Are Transforming Oncology Care
1. AI Wearables
AI-powered wearables are reshaping how oncologists monitor cancer patients by providing continuous, real-world data. Unlike traditional methods that depend on clinic visits every few weeks, these devices track vital metrics like heart rate, body temperature, oxygen levels (SpO2), and physical activity 24/7. The data is uploaded to the cloud within minutes, giving clinicians almost immediate access to patient health updates [8].
Real-Time Monitoring
One of the standout features of AI wearables is their ability to collect and analyze digital biomarkers - physiological signals that reveal a patient’s condition and symptom burden [3]. A report from Memorial Sloan Kettering Cancer Center, published in October 2024, showcased how three lung cancer patients (ages 55–71) were monitored using Apple Health data. Over 58 to 135 weeks, the system gathered between 34,319 and 103,535 physiological data points per patient, averaging around 41 measures daily. This continuous monitoring revealed changes in health that traditional ECOG scores might have missed.
AI algorithms excel at detecting anomalies, often identifying potential problems before patients even notice symptoms [3]. For instance, machine learning models using smartwatch data have achieved up to 93% accuracy in predicting mortality for end-of-life cancer patients [10]. These insights pave the way for more personalized care and better treatment management.
Treatment Adherence
AI wearables also play a key role in improving treatment adherence by offering personalized coaching and real-time feedback. Take the CAPRI trial, for example. This study involved 559 patients on oral anticancer medications and paired a nurse-led program with a smartphone app. Patients in the intervention group maintained a 93.4% relative dose intensity compared to 89.4% in the usual care group. They also experienced fewer severe toxicities and spent less time in the hospital [12].
"Patient-centered care through remote monitoring of symptoms and treatment may improve patient outcomes and experience." – Olivier Mir, Department of Ambulatory Cancer Care, Gustave Roussy [12]
Another study, the PATH trial at Johns Hopkins University, highlighted the impact of AI-guided interventions. In this trial, 42 overweight or sedentary cancer survivors used the AI voice-assisted "MyCoach" system, which integrated Fitbit Charge 2 HR data. Over four weeks, participants in the MyCoach group increased their daily step count by 3,568.9 steps (P < 0.001), compared to an increase of only 1,619 steps with basic text messaging. The system’s ability to provide personalized, two-way interaction significantly boosted adherence to physical activity [4].
Personalization
AI wearables don’t just track data - they use it to create highly individualized care plans. By analyzing patterns in sleep, activity, and medication adherence, these devices build a detailed health profile for each patient. This allows for timely, targeted interventions tailored to the individual’s needs [3][4].
"Wearable devices hold significant promise for the development of personalized 'digital biomarkers,' which may enhance risk stratification and management in oncology." – Joshua W. Bliss, New York Presbyterian, Weill Cornell Medicine [6]
Early Detection
The ability to detect subtle changes early is another major advantage of AI wearables. In the bwHealthApp pilot study, 31 gastrointestinal cancer outpatients at University Hospital Tübingen used wrist and in-ear devices between July and October 2022. These wearables collected over 20 million data points, including heart rate and temperature, in near real-time [8]. With this wealth of information, clinicians identified subtle physiological shifts that signaled potential hospitalizations or disease progression - issues that might have been overlooked during routine checkups. Additionally, a review of 199 studies found that more than 74% of patients adhered to wearable devices, showcasing their practicality [9].
At Healify, we’re taking this further by transforming wearable data into actionable insights. Our AI health coach, Anna, offers 24/7 personalized guidance, ensuring each patient gets support tailored to their unique health profile.
2. Standard Monitoring Methods
In traditional cancer care, patient progress is typically tracked through scheduled clinic visits. These appointments occur at set intervals during and after treatment [6]. At each visit, healthcare providers assess patients using subjective tools like the ECOG Performance Status and the Karnofsky Performance Status (KPS) to determine how well they can manage daily activities. They also analyze blood tests, imaging results, and cardiac evaluations to gauge overall health [6].
Real-Time Monitoring
The standard approach provides only periodic glimpses into a patient’s condition due to the infrequency of clinic visits [7]. Between these appointments, doctors rely heavily on patients' recollection of symptoms - a method often affected by recall bias. For instance, a study on advanced cancer patients revealed that those with a poor ECOG status (ECOG 3) averaged just 902 steps per day, compared to 5,345 steps for patients with a better ECOG status of 0 [7].
"Low sampling frequency due to periodic intervals of in-person visits during the treatment course further limits monitoring. Failure to detect early physiological symptoms contributes to suboptimal therapeutic management and poor clinical outcomes." – Frontiers in Oncology [6]
These constraints highlight the need for continuous, data-driven monitoring systems.
Treatment Adherence and Personalization
Tracking whether patients stick to their treatment plans is another challenge for standard monitoring methods. Relying on patients to recall and report their symptoms during visits often leads to underestimating symptom severity [3]. Additionally, static evaluations conducted before treatment fail to account for daily variations in a patient’s health, making it difficult to tailor care to their changing needs [6][7].
Early Detection
Traditional methods often miss critical early warning signs. A study conducted in October 2025 by researchers at Northwell Health's Feinstein Institutes examined 888 adult non-ICU inpatients. The findings showed that AI-powered continuous monitoring could predict patient deterioration an average of 17 hours earlier than standard intermittent vital sign checks. The AI system identified 83% of unplanned ICU transfers and successfully detected all cases of cardiac arrest or death within 24 hours [17].
"Currently, hospital staff rely on intermittent vital sign checks of a patient, like their heart rate or temperature, to identify worsening conditions. Combining clinical wearables with the predictive AI algorithm we have developed, we can help clinicians identify these deteriorations a lot earlier and more accurately than standard-of-care early warning scores." – Theodoros P. Zanos, PhD, Head of Northwell's Division of Health AI [17]
This inability to catch early signs of deterioration underscores the advantages of AI-driven wearables in providing timely and accurate patient insights.
Advantages and Disadvantages
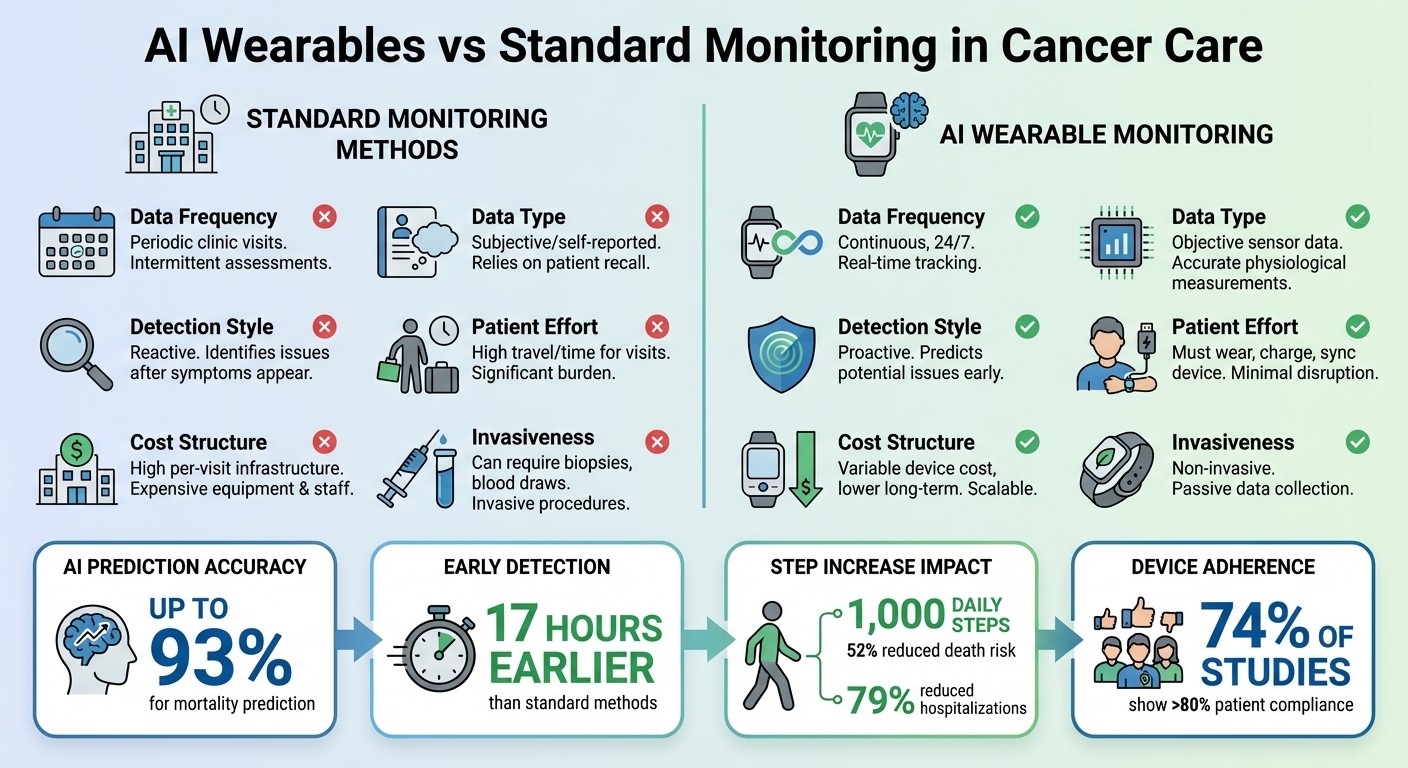
AI Wearables vs Standard Monitoring Methods in Cancer Care
When you stack AI wearables against traditional monitoring methods, the differences are striking. AI-driven devices provide round-the-clock data, while conventional methods depend on periodic snapshots during clinic visits. Wearables collect objective physiological data like heart rate variability and step counts, whereas traditional approaches often rely on self-reported information that can be skewed by memory lapses or biases [2]. This comparison shows how AI wearables address the gaps in accuracy and consistency seen in older methods.
AI systems also excel at predicting clinical outcomes. For instance, machine learning models have demonstrated impressive accuracy rates - up to 93% when analyzing medical images and 89% with smartwatch data [1][10]. In one study, advanced cancer patients who increased their daily steps by just 1,000 saw a 0.34 odds ratio for adverse events and a 48% reduction in death risk (HR: 0.48) [7].
That said, these devices aren’t without their challenges. Data privacy is a major concern due to the sheer volume of sensitive information being collected, which demands secure storage and regulated sharing [5]. There are also technical hurdles - sensors can be thrown off by motion distortions or environmental noise, and step counts might be less accurate for individuals with slower gaits [2][5]. Another issue is the "black box" nature of many AI models, which can make their decision-making processes less transparent and harder for clinicians to trust [1][21].
Feature | Standard Monitoring | AI Wearable Monitoring |
|---|---|---|
Data Frequency | Periodic clinic visits [10] | Continuous, 24/7 [6] |
Data Type | Subjective/self-reported [2] | Objective sensor data [2] |
Detection Style | Reactive [10] | Proactive [5] |
Patient Effort | High travel/time for visits [10] | Must wear, charge, sync device [20] |
Cost Structure | High per-visit infrastructure [10] | Variable device cost, lower long-term [10] |
Invasiveness | Can require biopsies, blood draws [10] | Non-invasive [5] |
While AI wearables clearly bring a host of benefits, there are barriers to widespread adoption. Digital literacy and access to reliable internet connectivity are key factors. These technologies often favor populations with strong digital skills and access to smartphones, potentially leaving others behind [1]. Older adults, in particular, may lack the devices or home internet needed for these wearables to work effectively [2]. On a positive note, adherence to these devices is high: over 80% of participants in 74% of studies reported consistent usage [9].
Conclusion
AI wearables are reshaping the landscape of cancer care by providing continuous, real-time health data. These devices offer a dynamic view of a patient’s condition, enabling early detection of potential issues and timely medical intervention.
Take the PATH trial at Johns Hopkins University as an example. Led by Ahmed Hassoon, this study explored the integration of AI with wearable technology. Cancer survivors who used the AI voice coach "MyCoach" increased their daily physical activity by an average of 3,568.9 steps over four weeks. This improvement significantly outpaced the results seen in control groups.
"AI-based voice-assisted coaching shows promise as a practical method of delivering scalable, individualized coaching to increase physical activity in sedentary cancer survivors" [4].
The implications of wearable data go beyond step counts. By leveraging this information, healthcare providers can refine treatment plans, better assess frailty, and predict chemotherapy tolerance more effectively than with traditional methods. Features like monitoring step counts as a vital sign and receiving automated alerts when thresholds are exceeded enable clinicians to act proactively [3][5].
However, there’s a notable gap in adoption - only 29% of cancer survivors currently use wearable activity trackers. Bridging this digital divide requires addressing barriers like access to devices, reliable internet, and digital literacy [11].
Pulling all this together, AI wearables are becoming indispensable in cancer care. They enhance treatment adherence and empower patients with tailored insights into their health. Platforms like Healify take this a step further, translating complex wearable data into actionable advice, ensuring cancer patients receive continuous support throughout their journey.
FAQs
How do AI-powered wearables help cancer patients stick to their treatment plans?
AI-powered wearables take raw health data - like heart rate, activity levels, sleep patterns, and medication schedules - and turn it into meaningful insights tailored to each individual. These devices analyze the information to spot missed doses, worsening symptoms, or noticeable changes in health. When something seems off, they send real-time alerts and practical advice to patients. With permission, they can also notify care teams, allowing for quick and effective interventions.
These wearables go a step further by offering custom medication reminders, predicting times when patients might struggle with adherence (like after chemotherapy), and adjusting coaching prompts to help users stay on track. Research shows that patients using these devices are more likely to follow their treatment plans, keep better tabs on their symptoms, and engage more with recommended activities - all of which contribute to better health outcomes. By blending constant monitoring with personalized support, these tools help patients stick to their therapy plans and take control of their health.
What are the challenges of using AI wearables in cancer care?
AI-powered wearables hold promise for reshaping cancer care, but they come with their own set of hurdles. One major challenge is integrating data from consumer-grade devices into clinical workflows. Aligning this data with medical-grade standards and meeting regulatory requirements can be a tricky process. On top of that, the constant transmission of sensitive health data raises serious privacy and security concerns, including issues around consent, data storage, and the risk of breaches.
Patient adherence is another significant obstacle. While many cancer patients start using wearables, they often abandon them due to discomfort, short battery life, or a lack of noticeable benefits. Socioeconomic factors also play a role - affordability and digital literacy can limit access to these technologies, leaving some populations behind. Furthermore, AI algorithms may generate biased or inaccurate results if they’re trained on datasets that don’t reflect diverse populations, which could unintentionally deepen health disparities.
Platforms like Healify are stepping up to tackle these challenges. By securely analyzing wearable data, they deliver personalized, actionable insights to users. With an emphasis on user-friendly design, clinical validation, and robust data security, solutions like Healify aim to make AI wearables more practical and accessible for improving cancer care.
How do AI wearables help detect health issues early for cancer patients?
AI-powered wearables are transforming personal health monitoring by tracking key metrics like heart rate, blood pressure, oxygen levels, sleep patterns, and activity levels - all in real time. These devices use AI to compare this data against personalized baselines, spotting subtle changes that might indicate potential health concerns before symptoms even surface. For instance, wearables have been used to identify early signs of infections in chemotherapy patients, helping to prevent serious cancer-related complications.
Beyond just detecting irregularities, these devices provide actionable alerts for both patients and their healthcare teams. Whether it's a warning about arrhythmias or early indicators of sepsis, these notifications can lead to timely interventions, ultimately reducing hospital visits and improving patient outcomes. Platforms such as Healify take this a step further by combining wearable data with health records and lifestyle information. This creates a 24/7 stream of personalized health insights, empowering patients and clinicians to address potential issues proactively.
Related Blog Posts
Finally take control of your health

Finally take control of your health

Finally take control of your health





